Tapering Schedule: How to Safely Reduce Medication Dosage
When you’ve been on a medication for weeks or months, your body adapts. Suddenly stopping can trigger withdrawal symptoms—shakiness, insomnia, nausea, or even seizures. A tapering schedule, a planned, gradual reduction in drug dosage to minimize withdrawal and maintain stability. Also known as drug tapering, it’s not optional for many drugs—it’s essential. This isn’t about cutting pills in half randomly. It’s about following a timeline designed for your specific medication, dose, and health history.
Some medications are more dangerous to quit cold turkey than others. Benzodiazepines, used for anxiety and sleep, can cause severe rebound anxiety or seizures if stopped too fast. Antidepressants, like SSRIs or SNRIs, often lead to brain zaps, dizziness, or mood crashes without a proper taper. Even common drugs like beta-blockers or steroids need careful reduction. The tapering schedule, a personalized plan that lowers dosage slowly over days, weeks, or months. The speed depends on the drug, how long you’ve taken it, and your body’s response. Some people need to drop 10% every two weeks. Others need months just to get off a single pill.
What makes a good taper? It’s not one-size-fits-all. If you’re switching from a brand drug to a generic, or moving from one class of meds to another, your taper might need adjusting. That’s why monitoring your symptoms matters. Did your sleep get worse after a small cut? Did your anxiety spike? These aren’t just inconveniences—they’re signals your body needs more time. Doctors use tools like the Beers Criteria for seniors or pharmacogenomic data to tailor plans, especially when dealing with complex cases like opioid dependence or epilepsy meds.
Many people think tapering is just about cutting pills. It’s not. It’s about timing, support, and knowing when to pause. Some people need to hold at a dose for weeks before going lower. Others need to switch to a longer-acting version first. And if you’re on multiple drugs—say, an antidepressant and a sleep aid—you might need to taper one at a time. The goal isn’t just to stop the drug. It’s to stop safely, without losing the progress you’ve made.
Below, you’ll find real-world guides on how to handle medication changes without risking your health. From benzodiazepine withdrawal in seniors to managing antidepressant side effects during a taper, these posts give you the facts—not guesses. Whether you’re a patient, caregiver, or just trying to understand why your doctor won’t let you quit cold turkey, you’ll find clear, practical advice here.
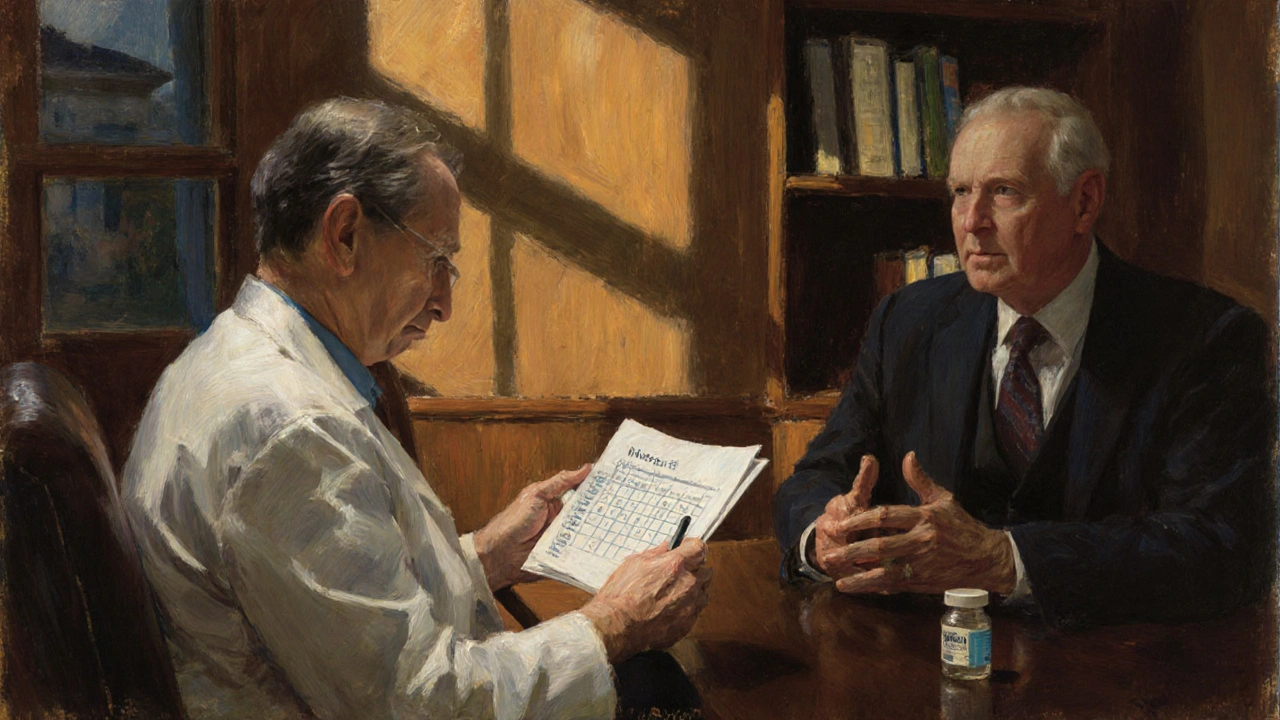
How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
Learn how to safely talk to your doctor about stopping or tapering a medication. Get clear steps, expert-backed tapering schedules, and communication tips to avoid withdrawal and stay in control of your health.
Read more