Stopping a medication isn’t as simple as just skipping a pill. For many drugs-especially antidepressants, benzodiazepines, and opioids-suddenly quitting can trigger serious withdrawal symptoms like anxiety, insomnia, dizziness, nausea, or even seizures. Even if you feel fine, your body may have adapted to the drug’s presence. That’s why medication tapering-gradually lowering your dose over time-is often the safest way to stop. But here’s the catch: no one can do it right unless you and your doctor talk openly, honestly, and together.
Why You Can’t Just Quit Cold Turkey
Your body doesn’t treat all medications the same. Some, like ibuprofen or antibiotics, can be stopped without issue. Others, like SSRIs (e.g., sertraline, escitalopram), benzodiazepines (e.g., alprazolam, clonazepam), or opioids (e.g., oxycodone, hydrocodone), cause physical dependence. That means your brain and nervous system have adjusted to their presence. When you remove them too fast, your system goes into shock. A 2021 review in the Journal of Clinical Psychiatry found that 8-12% of people who stop long-term benzodiazepines abruptly experience severe withdrawal. For antidepressants, nearly 1 in 3 patients report moderate to severe symptoms like brain zaps, flu-like feelings, or mood crashes when they quit too quickly. Opioid withdrawal isn’t usually life-threatening, but it’s intensely uncomfortable-sweating, cramps, diarrhea, and intense anxiety-that often drives people back to using. The good news? These symptoms are preventable. Studies show that structured tapering reduces emergency room visits by 37% and improves completion rates by more than double compared to unguided stops. But none of that matters if you don’t have the right conversation with your provider.What Your Doctor Needs to Know Before Tapering
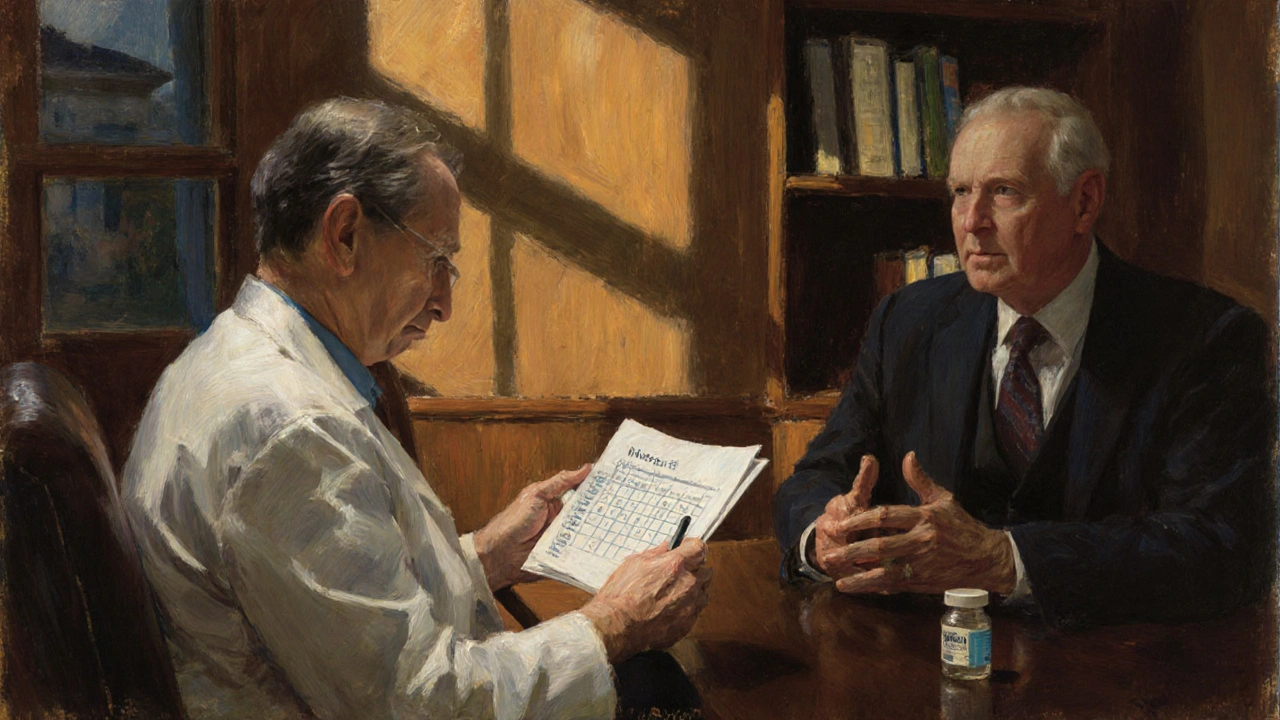
Your doctor isn’t just looking at your prescription bottle. They need to understand your whole picture. Before even suggesting a taper, they should ask:- Why are you considering stopping? (Side effects? Feeling better? Worried about long-term use?)
- How has this medication affected your daily life? (Sleep? Mood? Pain? Energy?)
- Have you ever tried stopping before? What happened?
- Are you taking other medications or substances? (Alcohol, sleep aids, pain meds?)
How to Start the Conversation
Don’t wait for your appointment to bring it up. Send a quick message or note before your visit: > “I’ve been thinking about reducing my [medication name]. I’d like to talk about whether a taper might be safe for me, and what that could look like.” That simple sentence opens the door. During the appointment, use these phrases to guide the discussion:- “Can you explain why this medication was prescribed in the first place?”
- “What are the risks if I stop too quickly?”
- “What does a safe taper look like for someone like me?”
- “How will we know if I’m going too fast?”
- “Can we write this plan down?”
What a Safe Tapering Plan Actually Looks Like
There’s no one-size-fits-all schedule. Taper speed depends on the drug, how long you’ve taken it, your metabolism, and your symptoms. Here’s what evidence-based guidelines suggest:- Benzodiazepines: For people on it longer than 6 months, reduce by 5-10% every 1-2 weeks. A full taper can take 4-26 weeks. Fast tapers increase withdrawal risk by 40-60%.
- Opioids: Mayo Clinic recommends reducing by 10% of your original dose every 5-7 days until you hit 30% of the original dose, then slowing to 10% weekly. For some, this takes 8-12 weeks.
- Antidepressants: SSRIs like fluoxetine (Prozac) have long half-lives and can be tapered in 1-2 weeks. Others, like paroxetine (Paxil), need 4-8 weeks. Some patients benefit from using specialized liquid or cuttable tablets to make tiny reductions.
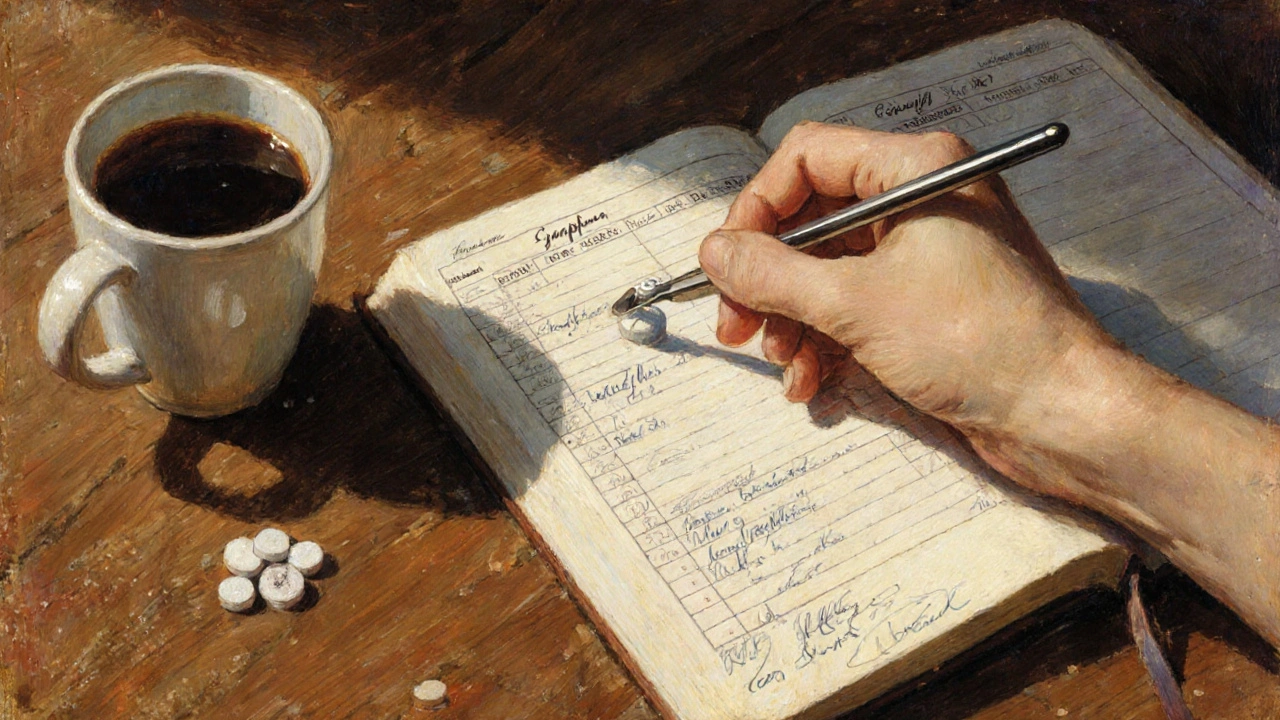
How to Monitor Symptoms During a Taper
You won’t feel withdrawal right away. Symptoms often appear 2-7 days after a dose reduction. Keep a simple log:- Date of dose change
- Current dose
- Any new symptoms (anxiety, headaches, sleep issues, nausea)
- How those symptoms affect your day (mild, moderate, severe)
- Any changes in mood or energy
When to Pause or Slow Down
A good taper isn’t rigid. It’s responsive. If you start having moderate-to-severe symptoms, you’re going too fast. That doesn’t mean you failed. It means your body needs more time. The American Society of Addiction Medicine recommends pausing the taper for 1-2 weeks if symptoms become disruptive. Then, restart at a slower pace. Some patients need to hold at a dose for months before continuing. That’s normal. One patient on Reddit shared: “My doctor told me to cut 10% every week. Week 3, I couldn’t sleep or focus. I panicked and went back to my old dose. I felt betrayed.” That’s what happens when there’s no plan for setbacks. A strong provider will say, “Let’s hold here for two weeks. We’ll try 5% next time.”What to Do If Your Doctor Pushes You to Quit Fast
Not all providers are trained in tapering. Some still believe patients “should just get off it.” Others are pressured by insurance or guidelines that push for rapid reductions. If your doctor says, “You’ve been on this too long-let’s cut it in half next week,” push back. Ask:- “What’s the evidence for this speed?”
- “Are you following ASAM or CDC guidelines?”
- “Can I get a written plan with specific percentages and timelines?”

What Success Looks Like
Success isn’t just stopping the medication. It’s stopping without trauma. Patients who report the best outcomes say their doctors:- Explained the “why” using their own health data
- Created a written plan they could keep
- Allowed them to control the pace within safe limits
- Checked in weekly at first
- Offered support for symptoms (like sleep aids or therapy referrals)
What Comes After the Taper
Stopping the medication is only half the journey. After you’re off, you still need support. Withdrawal symptoms can linger for weeks or even months. Mood swings, sleep issues, or brain fog may continue. That doesn’t mean you’re relapsing-it means your brain is rewiring. Ask your provider:- “What should I expect in the next 4-8 weeks?”
- “Are there non-medication strategies to help with lingering symptoms?”
- “Should I schedule a check-in in 30 or 60 days?”

Sue Barnes
November 27, 2025 AT 10:49Ugh, another one of those "just talk to your doctor" articles. Like they actually care. My psychiatrist told me to cut my SSRIs in half in two weeks and laughed when I said I felt like I was being pulled apart from the inside. You think you're being heard? Nah. You're just a number on their quota sheet.
And don't even get me started on "written plans." I asked for one. Got a one-page PDF with bullet points and a link to a 300-page NIH study. That's not a plan. That's a middle finger with footnotes.
jobin joshua
November 28, 2025 AT 05:15Broooo this hit different 😭 I tapered off clonazepam last year and it felt like my brain was a broken Wi-Fi router trying to reconnect to a server that shut down. Took 14 weeks. My doc didn’t even know about the 5-10% rule. I had to Google it myself. 🙃
Now I’m off it and I sleep like a baby. But man, those first 3 weeks? I cried watching cartoons. Not even joking.
Sachin Agnihotri
November 29, 2025 AT 08:12Really appreciate this breakdown-so many people don’t realize how dangerous cold turkey is, especially with benzos. I’ve seen friends go through it and it’s terrifying. One guy thought he could just stop his 10mg of sertraline because "he felt fine," and ended up in the ER with vertigo and panic attacks for three days.
But here’s the thing: even when you know the science, doctors still rush you. I had mine push me to cut 20% weekly because "insurance doesn’t cover long-term follow-ups." That’s not care. That’s cost-cutting dressed up as medicine.
Always ask for the written plan. Always. And if they say "you’ll be fine," ask them if they’d do it to their kid. If they hesitate? Walk out.
Diana Askew
November 30, 2025 AT 06:06They don’t want you off the meds because Big Pharma owns the FDA. You think this is about your health? No. It’s about profits. They need you hooked. That’s why they make tapering sound so complicated-so you’ll stay on it.
Also, did you know that 78% of doctors get paid by drug companies? I read it on a blog. It’s true. Don’t trust them. Ever.
And why do they always say "brain zaps" like it’s some weird myth? I had them. They felt like electric shocks in my skull. They’re real. They’re not "in your head."
Also, your doctor probably doesn’t even know what a half-life is. Don’t believe the hype. The truth is hidden. Always.
King Property
November 30, 2025 AT 10:18Look. You people are overcomplicating this. If you’re on antidepressants for more than 6 months, you’re probably just lazy. Your brain doesn’t need a 26-week taper. It needs a kick in the ass.
I quit my SSRI cold turkey in 2018. Felt weird for 4 days. Got over it. Now I’m healthier than ever. You want to feel better? Stop being a baby. Stop asking for permission. Just stop.
And if your doctor won’t let you? Find a new one. Or better yet-stop taking their advice. You’re an adult. Act like one. No one’s stopping you from throwing out your pills. Except you.
Yash Hemrajani
November 30, 2025 AT 16:13Oh wow, a whole article on tapering and not a single mention of the fact that 90% of people who taper successfully do it because they had a damn good therapist helping them, not because their doctor gave them a spreadsheet.
Doctors don’t have time. They’ve got 12 patients an hour. You think they’re gonna sit there and walk you through liquid sertraline dosing? Nah. You need a therapist who knows withdrawal symptoms like the back of their hand.
And yes, I’ve been there. I’ve held people’s hands through brain zaps. You don’t need a doctor. You need someone who’s been there. Find that person. Not the one with the MD after their name.
Pawittar Singh
December 2, 2025 AT 11:57Y’all are killing me with the drama 😊 I know it’s scary-I’ve been there too. But here’s the thing: you’re not alone. Seriously. There are thousands of us who’ve tapered, survived, and now feel more alive than ever.
My doc didn’t get it at first. So I printed out the ASAM guidelines and handed them to him. He said, "I didn’t know this existed." Now he uses it for everyone.
Don’t give up. Don’t let the fear win. You’re stronger than your meds. And if you’re reading this? You’re already doing better than you think.
And if you need someone to talk to? DM me. I’ll reply at 2am. I’ve been up with the zaps. I get it. 💪❤️
Josh Evans
December 3, 2025 AT 15:18I really liked this. I tapered off gabapentin after 3 years and it was brutal, but having a written schedule made all the difference. My doctor actually sat down with me and we made a chart. I marked off each week. It felt like a victory log.
Also, keeping a symptom journal helped me realize that the worst days weren’t right after the cut-they came 3-4 days later. That helped me not panic.
Biggest takeaway: you’re not weak for needing a plan. You’re smart.
Allison Reed
December 4, 2025 AT 06:27This is exactly the kind of clear, compassionate, evidence-based guidance people need. Too many patients are left to navigate tapering alone, which is dangerous and deeply unfair.
I’ve worked in mental health for over a decade, and the most successful outcomes always involve collaboration, patience, and documentation. The fact that this article emphasizes writing down the plan and tracking symptoms? That’s gold.
Also, the point about asking for a referral if your doctor isn’t trained? Spot on. You deserve care that respects your biology-not your insurance provider’s bottom line.
Jacob Keil
December 4, 2025 AT 13:24so like… if your brain adapts to the drug… then when you stop… its like… your brain is like… "wait where did the chemicals go?" and it panics right? like… its not you being weak… its just… biology being biology?
but then why do some people just stop and be fine? is it just… luck? or… is it because their brain was never really adapted? or… maybe they were on it too short?
i dont know. i think the whole thing is a metaphysical mystery. we think we control our minds but really… the pills control us. or maybe… we control the pills? idk. just thinking out loud. lol
Rosy Wilkens
December 6, 2025 AT 05:02As a former pharmaceutical representative, I can tell you this article is dangerously misleading. The entire tapering narrative is a myth perpetuated by the mental health industry to prolong dependency. Most patients who claim withdrawal symptoms are simply experiencing rebound anxiety or depression-conditions they had before they ever took the medication.
The CDC guidelines? Politically motivated. The ASAM? Funded by addiction treatment centers with a vested interest in keeping people in treatment. You think your doctor is helping you? They’re being paid by the same companies that manufacture these drugs to keep you on them indefinitely.
Stop listening to this pseudoscience. The only way to be free is to quit cold turkey. Your body will adapt. It always does. The real issue? Your lack of willpower.