Stopping Medication Safely: How to Quit Drugs Without Risk
When you decide to stop taking a medication, you're not just ending a habit—you're changing how your body functions. Stopping medication safely, the careful, guided process of reducing or ending drug use to avoid harm. Also known as deprescribing, it's not about willpower—it's about biology. Many people think if a drug isn't working anymore, they can just quit. But that’s how seizures, panic attacks, high blood pressure spikes, and even heart problems start. Some meds, like antidepressants or benzodiazepines, need to come off slowly—sometimes over weeks or months. Others, like insulin or blood thinners, can be deadly if stopped cold. The body adapts. When you remove the drug, it has to readjust, and that’s where things go wrong if you don’t plan it right.
Not all drugs are the same when it comes to quitting. Benzodiazepines, a class of drugs used for anxiety and sleep, often prescribed long-term to seniors, can cause severe withdrawal symptoms like tremors, hallucinations, or seizures if stopped abruptly. That’s why doctors now recommend tapering them slowly, especially in older adults. Antidepressants, medications that alter brain chemistry to lift mood, can trigger dizziness, brain zaps, nausea, or rebound anxiety—even if you’ve been on them for just a few weeks. And even common drugs like beta-blockers for blood pressure or steroids for inflammation can cause dangerous rebounds if pulled too fast. This isn’t theoretical. Studies show over 30% of people who stop antidepressants cold report moderate to severe withdrawal, and many end up back on the drug because they didn’t know how to quit.
What you need to know is this: stopping safely isn’t about speed. It’s about control. It means talking to your doctor before you make a move, tracking symptoms as you reduce, and knowing what’s normal versus what’s a red flag. It also means understanding that generics aren’t always interchangeable when you’re tapering—some people notice differences in how they feel when switching from brand to generic during withdrawal. And if you’re on multiple meds, interactions can make withdrawal worse. That’s why reading your prescription labels and knowing your drug interactions matters, even when you’re trying to stop.
There’s no one-size-fits-all plan. What works for someone quitting a sleep aid won’t work for someone coming off an anti-seizure drug. But the principles are the same: slow, steady, and supervised. You don’t need to suffer through withdrawal. You don’t need to guess. You just need the right information—and that’s what you’ll find below. From real stories about tapering off antidepressants to how to spot early signs of withdrawal from pain meds, these posts give you the tools to quit drugs without risking your health.
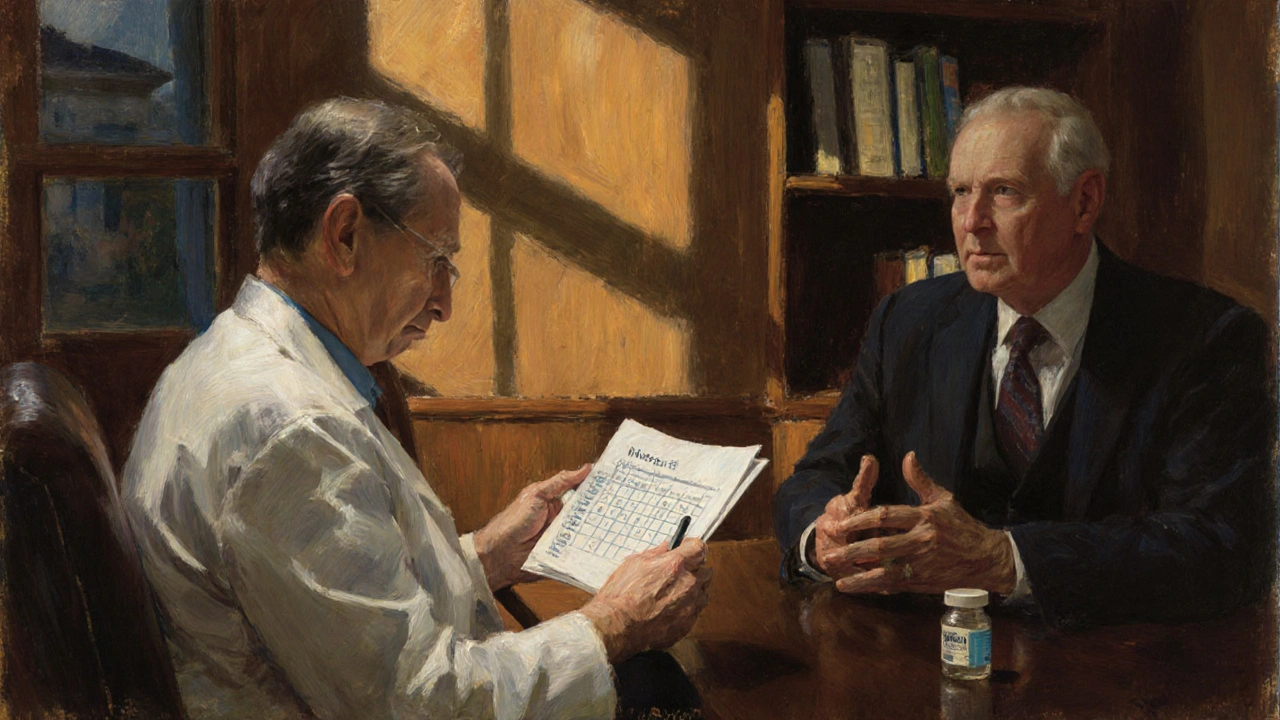
How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
Learn how to safely talk to your doctor about stopping or tapering a medication. Get clear steps, expert-backed tapering schedules, and communication tips to avoid withdrawal and stay in control of your health.
Read more