Medication Withdrawal: What Happens When You Stop Taking Your Drugs
When you stop taking a medicine your body has gotten used to, you might not feel right—sometimes badly. This is called medication withdrawal, the physical and mental reactions that happen after stopping a drug your system has adapted to. It’s not just "feeling off." It’s your nervous system, hormones, and brain chemistry readjusting after being altered by the drug for weeks, months, or years. This isn’t the same as addiction, though the two can overlap. Many people think withdrawal only happens with illegal drugs or opioids, but it’s common with antidepressants, blood pressure pills, steroids, even antihistamines and acid reducers.
Discontinuation syndrome, a specific set of symptoms that occur after stopping certain medications abruptly is real and well-documented. For example, people stopping SSRIs like sertraline or escitalopram often report dizziness, electric-shock sensations, nausea, or insomnia. Those quitting benzodiazepines may face anxiety spikes, tremors, or even seizures. Even stopping a daily painkiller like gabapentin can cause rebound pain or restlessness. The severity depends on the drug, how long you took it, and how fast you stopped. Some people barely notice anything. Others end up in the ER. That’s why tapering off meds, gradually reducing the dose under medical supervision isn’t optional—it’s essential for safety.
What you might not realize is that withdrawal symptoms can show up days or even weeks after your last pill. That’s why many think their new headache or sleep trouble is unrelated. But if you recently changed or stopped a drug, it’s worth considering. Some drugs, like antidepressants and anticonvulsants, have short half-lives, meaning they leave your system fast—and your body reacts fast. Others linger longer, but still trigger delayed withdrawal. And here’s the catch: if you’ve ever switched from brand to generic, or had an insurance denial that forced a drug change, you might’ve gone through withdrawal without even knowing it. That’s why withdrawal management, a planned, monitored process to reduce or stop medication safely matters more than most doctors admit.
You’ll find real stories below—people who felt awful after stopping their meds, how they recovered, and what they wish they’d known. There’s advice on spotting early signs, which drugs are riskiest, and how to talk to your doctor without sounding paranoid. You’ll also see how switching generics can trigger withdrawal-like reactions, why some people need months to taper, and what to do if your pharmacy runs out of your drug. This isn’t about fear. It’s about control. You don’t have to guess what your body is doing. There are clear steps. You just need to know where to look.
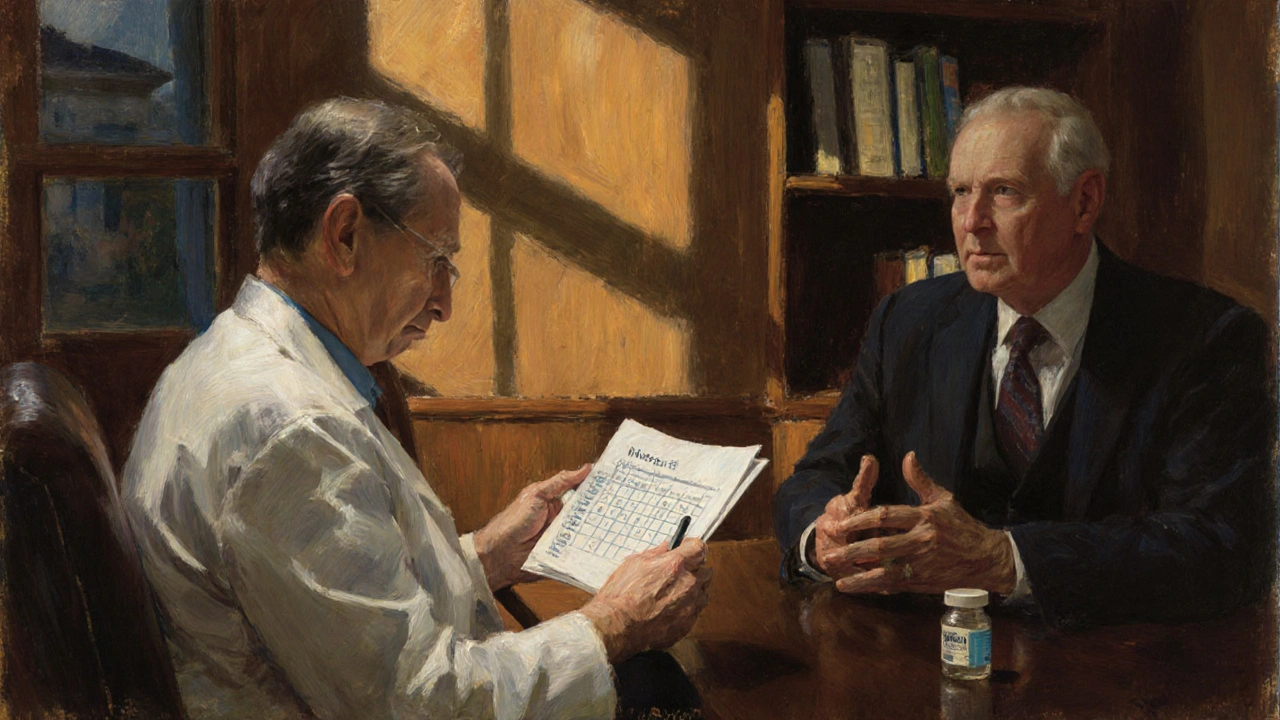
How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
Learn how to safely talk to your doctor about stopping or tapering a medication. Get clear steps, expert-backed tapering schedules, and communication tips to avoid withdrawal and stay in control of your health.
Read more