Insurance Appeal Generic: How to Fight Denials for Generic Medications
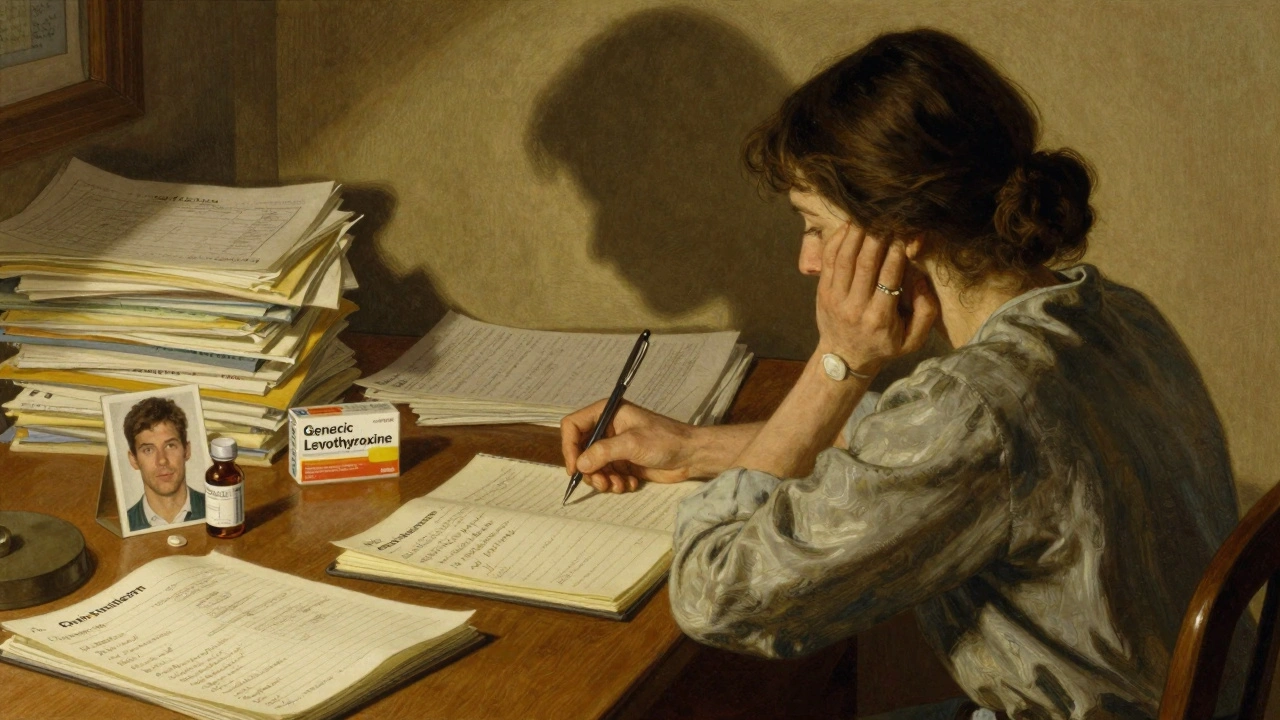
When your insurance refuses to cover a generic drug, a lower-cost version of a brand-name medication approved by the FDA as equally safe and effective. Also known as generic medication, it’s often the go-to choice for pharmacies and patients looking to cut costs without losing effectiveness. But if your plan denies it—maybe they want the brand version, or they say it’s "not medically necessary"—you’re not stuck. You can fight back. Insurance appeal generic requests work more often than people think, especially when you know what to say and what documents to send.
Most denials happen because of formulary rules, prior authorization steps, or tiered pricing. Your plan might list a brand-name drug as preferred, even if the generic costs 80% less and works the same. That’s not always medical—it’s financial. But the law doesn’t let insurers play games. If your doctor says the generic is appropriate, and it’s FDA-approved, you have a strong case. You’ll need a letter from your prescriber explaining why the generic is right for you, proof of prior denials, and a clear copy of your plan’s coverage policy. Some people win by simply asking: "Why is the more expensive option being forced on me when the cheaper one is identical?" It’s not rude—it’s smart.
Related issues often come up with authorized generics, the exact same drug as the brand, made by the same company but sold under a generic label. These are sometimes overlooked in appeals because they look like brand-name drugs on paper. If your doctor says you react poorly to regular generics but do fine with the brand, ask for the authorized version—it’s still cheaper than the original brand and often covered under generic tiers. And if you’re on Medicare Part D, coverage gaps and tier changes can trigger denials too. You’re not alone if you’ve had to call your insurer three times, fill out three forms, and wait weeks for an answer. That’s why having a system matters: keep records, note dates, and follow up in writing.
Don’t assume your insurance knows what’s best. They’re focused on cost, not your experience. But you have rights. The process isn’t magic—it’s paperwork, persistence, and knowing the right questions to ask. Below, you’ll find real stories and step-by-step guides from people who’ve successfully overturned denials for generic medications. Some fought for asthma meds, others for blood pressure pills or epilepsy drugs. Each case was different, but the strategy was the same: be clear, be calm, and be ready with proof. You don’t need a lawyer. You just need to know what to say.
Insurance Appeals: Fighting Denials When a Generic Medication Doesn't Work
When generic medications fail, insurance often denies coverage. Learn how to fight back with proven steps, real examples, and free resources to get your brand-name drug approved.
Read more