When Your Generic Medication Doesn’t Work, Insurance Won’t Always Help
You’ve been told your brand-name drug is too expensive, so your doctor switched you to a generic. But within weeks, your symptoms came back worse than before. Your seizures returned. Your thyroid levels went haywire. You felt dizzy, anxious, or just plain worse. You call your insurance company to ask for your original medication back. They say no. Generic is cheaper. It’s FDA-approved. It’s bioequivalent. End of story.
But here’s the truth: bioequivalent doesn’t mean identical. And for some people, that small difference can be life-changing.
Why a Generic Might Fail When It’s Supposed to Work
The FDA says generics must deliver 80% to 125% of the active ingredient compared to the brand-name version. That sounds precise-until you realize that for drugs like levothyroxine, warfarin, or epilepsy meds, even a 5% shift can trigger dangerous side effects or treatment failure.
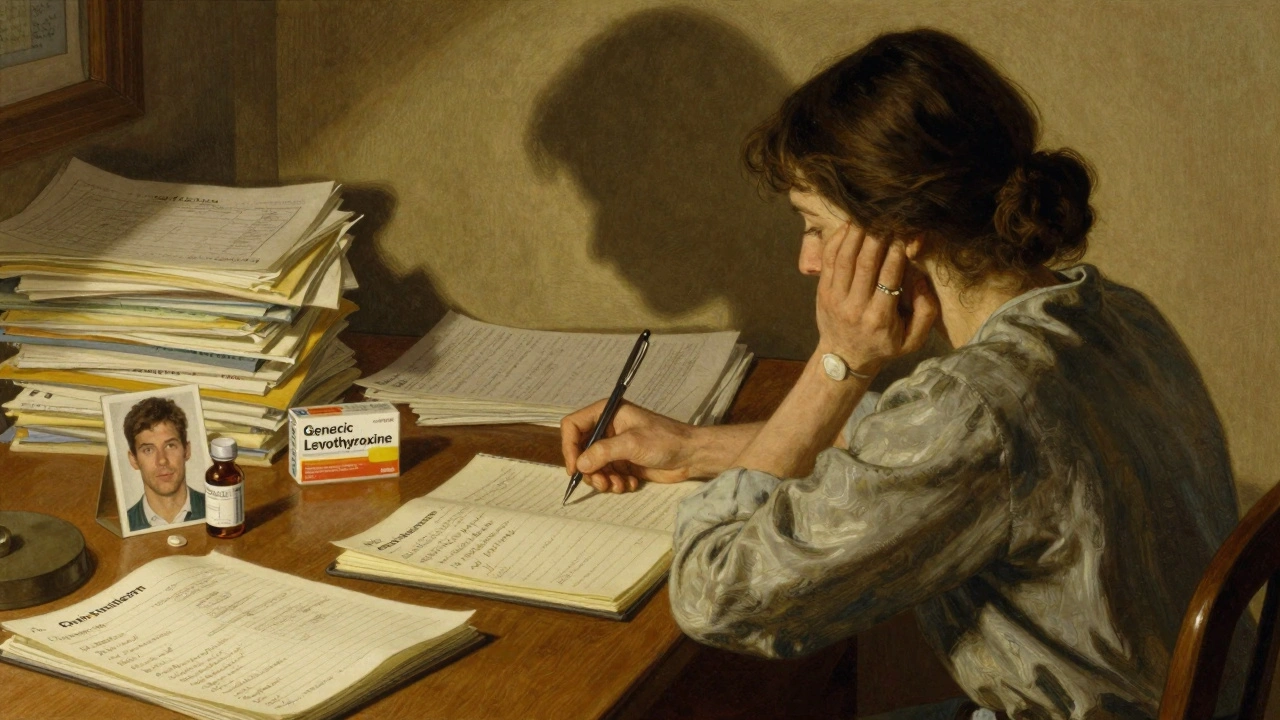
Take Synthroid, for example. It’s a brand-name thyroid medication. Many patients switch to generic levothyroxine without issue. But for others, their TSH levels spike from 2.1 to 14.7 after the switch. Why? It’s not about the active ingredient-it’s about the fillers, binders, and coating. Different manufacturers use different inactive ingredients. For people with autoimmune thyroid disease, those additives can interfere with absorption. One study showed nearly 20% of patients on narrow-therapeutic-index drugs experience measurable clinical differences when switching to generics.
It’s not just thyroid meds. People with epilepsy report breakthrough seizures after switching from Keppra to generic levetiracetam. Patients on warfarin see their INR levels swing unpredictably. And for those with chronic pain or mental health conditions, subtle changes in how the drug is absorbed can make the difference between functioning and being bedridden.
Insurance Doesn’t Care-Until You Make Them
Insurance companies don’t deny coverage because they’re cruel. They deny it because they’re incentivized to. Generics make up 90% of prescriptions but only 23% of drug spending. For them, pushing generics is a cost-saving machine. But that machine doesn’t account for individual biology.
When you get denied, you’re not just fighting a policy. You’re fighting a system designed to assume everyone responds the same way. That’s where the appeal process comes in. And yes, it’s complicated. But it works-if you do it right.
How to Win Your Appeal: The 5 Steps That Actually Matter
Most people give up after the first denial. But according to the Patient Advocate Foundation, 67% of appeals that go to external review are approved-when they have the right documentation.
- Get your Explanation of Benefits (EOB)-right away. Look for denial codes like DA2000 (generic available) or DA1200 (not on formulary). Write them down. These are your battle lines.
- Document everything. Keep a daily log: what time you took the generic, what symptoms you had, how bad they were. Take photos of your journal if you need to. Don’t wait until your appointment-start now.
- Get your doctor to write a letter. Not a note. A letter. It needs to say: “Patient experienced therapeutic failure with generic [drug name]. Symptoms returned or worsened. Lab results show [TSH, INR, seizure frequency, etc.] moved outside therapeutic range. Brand-name [drug name] is medically necessary.” Include ICD-10 codes. Reference guidelines like the Endocrine Society’s 2019 thyroid recommendations. The more specific, the better.
- Include lab results. A single blood test won’t cut it. Show the trend: pre-generic levels, post-generic levels. If your TSH jumped from 2.1 to 14.7 over 8 weeks, that’s not coincidence. That’s evidence.
- Submit your appeal within the deadline. For commercial insurance, you have 180 days. For Medicare Part D, you have 60. Miss it, and you lose your right to appeal.
Don’t rely on your doctor to do it all. Bring your logs and lab reports to your appointment. Say: “I need you to write a letter for my insurance appeal. Here’s what happened. Can you help?” Most doctors will. If they hesitate, ask if they’ve done this before. Many have.
What Works Best: Real Examples from People Who Won
A patient in Melbourne with a SCN1A gene mutation was switched from brand-name Keppra to generic levetiracetam. Within weeks, she developed severe neuropsychiatric side effects-hallucinations, aggression. Her neurologist submitted an appeal with functional MRI scans showing abnormal brain activity only after the switch. Approved on the first external review.
Another patient, diagnosed with Crohn’s disease, tried three different biosimilars after his brand-name biologic was denied. Each one caused flare-ups. His appeal included dates, dosages, and hospital visits. Approved after the second external review.
On Reddit, a user named u/ThyroidWarrior shared his story: after switching to generic levothyroxine, his TSH skyrocketed. He brought his lab results to his endocrinologist, who wrote a letter citing the Endocrine Society’s guidelines. His insurer approved the brand-name drug within 11 days.
What Doesn’t Work: The Mistakes That Cost People Their Medication
“I’ve been on this generic for months and it’s fine.” - That’s not proof of failure. You need to show the change happened after the switch.
“My doctor says it’s better.” - Vague statements like this get rejected. You need data.
Waiting too long to act. One man waited six months after his seizures returned before filing. By then, he’d had two ER visits and lost his job. He appealed anyway-but he could’ve avoided it all.
And here’s the worst one: letting your doctor write a one-sentence note. “Patient needs brand-name drug.” That’s not enough. Insurance sees hundreds of these. They ignore them.
State Rules and Medicare: Know Your Leverage
In California, New York, and Texas, appeals for therapeutic failure have a 63% success rate. Why? Those states require insurers to consider individual patient response-not just lab numbers.
Medicare Part D has a five-step appeal process. The first level is fast: 7 days for standard, 72 hours for urgent cases. And since the Inflation Reduction Act, if you win, you don’t pay anything for the drug during the appeal.
Twenty-eight states now ban “step therapy” for documented therapeutic failure. That means insurers can’t force you to try three generics before approving your brand-name drug. If they do, it’s illegal.
Help Is Out There-And It’s Free
You don’t have to do this alone.
GoodRx’s Appeal Assistant walks you through a template letter. Over 147,000 people used it in 2023. It’s free. It’s simple. Your doctor just signs it.
The Patient Advocate Foundation offers free case managers. Call 1-800-532-5274. They’ve helped over 12,000 people appeal drug denials. Their success rate? 67%.
Non-profits like the Crohn’s & Colitis Foundation and the Epilepsy Foundation have downloadable appeal toolkits. They include sample letters, lab form templates, and state-specific rules.
The Bigger Picture: Why This Matters
This isn’t just about one pill. It’s about whether your healthcare system sees you as a person-or a cost center.
Every year, $28 billion is spent on hospitalizations because people couldn’t get the right medication. That’s avoidable. That’s preventable. And every successful appeal pushes the system a little closer to recognizing that biology isn’t one-size-fits-all.
Doctors are speaking up. The FDA is considering new guidance on individualized bioequivalence. Employers are starting to require their pharmacy benefit managers to allow therapeutic exceptions. Change is slow-but it’s happening.
What to Do Next
If you’re reading this because your insurance denied your brand-name drug, here’s your action plan:
- Grab your EOB today.
- Start your symptom log-today.
- Call your doctor’s office and ask for a 30-minute slot just to talk about your appeal.
- Download the GoodRx Appeal Assistant or call the Patient Advocate Foundation.
You don’t need to be a medical expert. You just need to be persistent. And you’re not alone.
What if my insurance says the generic is just as good?
Insurance companies often use boilerplate language like “bioequivalent = clinically equivalent.” But that’s not true. Bioequivalence means the drug is absorbed at a similar rate in healthy people under lab conditions. It doesn’t account for individual differences in metabolism, gut health, or autoimmune conditions. Your appeal must show real-world failure-symptoms, lab results, and doctor confirmation.
How long does an appeal take?
Internal appeals take 14-30 days. External reviews take 30-45 days. For urgent cases-like seizures, unstable thyroid levels, or suicidal depression-you can request an expedited review. Medicare must respond in 72 hours. Commercial insurers must respond within 72 hours if your condition could be seriously harmed by delay.
Can I switch back to the brand-name drug if I win?
Yes. Once approved, your insurance must cover the brand-name drug for as long as your doctor says it’s medically necessary. You may need to re-apply annually, but your approval sets a precedent. Some insurers will even keep you on the brand-name drug indefinitely if you’ve proven it’s the only option that works.
What if I can’t afford the brand-name drug even after approval?
Many drug manufacturers offer patient assistance programs. For example, AbbVie (maker of Humira) and Takeda (maker of Entyvio) have free drug programs for qualifying patients. GoodRx also has coupons that can reduce out-of-pocket costs by up to 80%. And under Medicare, if you win your appeal, you pay nothing for the drug during the appeal period.
Do I need a lawyer?
No. Most appeals are won without legal help. The key is documentation, not legal jargon. However, if your appeal is denied at the external review level and you’re on Medicare, you can request a hearing with an administrative law judge. That’s when a lawyer can help-but only after exhausting all other options.
Can my pharmacist help?
Yes. Pharmacists are trained in medication therapy management. Ask yours to document any changes in your symptoms after a generic switch. Many pharmacies now include these notes in your file. These notes can be attached to your appeal and carry significant weight.

Joanne Rencher
December 4, 2025 AT 01:37Adrianna Alfano
December 6, 2025 AT 00:57Casey Lyn Keller
December 6, 2025 AT 18:16Stacy Natanielle
December 7, 2025 AT 13:28kelly mckeown
December 8, 2025 AT 17:56Tom Costello
December 10, 2025 AT 08:20dylan dowsett
December 12, 2025 AT 00:22Chad Kennedy
December 12, 2025 AT 19:03Siddharth Notani
December 13, 2025 AT 14:05Cyndy Gregoria
December 13, 2025 AT 15:40Akash Sharma
December 14, 2025 AT 14:49Justin Hampton
December 16, 2025 AT 13:23