Hormone Disruption: Causes, Signs, and How It Affects Your Health
When your body’s hormone disruption, a condition where natural hormone levels are thrown off by external or internal factors. Also known as endocrine disruption, it doesn’t always show up as a diagnosis—but it shows up in your sleep, your mood, and your waistline. It’s not just about menopause or thyroid problems. It’s also about the plastics in your food containers, the chemicals in your lotion, the stress that keeps your cortisol high, and the medications that accidentally mess with your natural balance.
Think about estrogen imbalance, when estrogen levels are too high or too low compared to other hormones like progesterone. That’s what drives hot flashes, weight gain around the belly, and even mood crashes—something many women notice after switching birth control or during perimenopause. But men get it too. Low testosterone isn’t just aging—it can be triggered by exposure to endocrine disruptors, chemicals like BPA, phthalates, and parabens that mimic or block hormones. These show up in canned foods, plastic wrap, even some cosmetics. And they don’t need to be in large doses to cause trouble. Small, daily exposure adds up.
Then there’s cortisol stress, the body’s main stress hormone that, when chronically elevated, suppresses thyroid function and insulin sensitivity. If you’re always tired, always hungry, or always anxious, cortisol might be running the show. It doesn’t just come from work. Poor sleep, sugar crashes, and even too much caffeine can keep it stuck on high. And when cortisol is high, your thyroid slows down—leading to weight gain, brain fog, and cold hands. That’s why people feel fine on paper but awful in real life.
And let’s not forget your thyroid. Even if your doctor says your TSH is normal, you might still be struggling with thyroid function, the process by which your thyroid gland produces hormones that control metabolism, energy, and body temperature. Autoimmune issues, iodine deficiency, and environmental toxins can all interfere. Many of the posts below show how medications—like antidepressants or birth control—can indirectly mess with these systems. One person’s sweating problem might be tied to estrogen shifts. Another’s weight gain might be from thyroid slowdown triggered by a generic drug change.
This isn’t about panic. It’s about awareness. You don’t need to live in a glass bubble to protect yourself. You just need to know what to look for: unexplained fatigue, sudden weight changes, mood swings that don’t match your life, sleep that feels broken even when you’re tired. The posts here don’t just list symptoms—they connect the dots between everyday meds, lifestyle choices, and hidden hormone triggers. Whether it’s how vitamin B6 helps with stress, why switching generics can change your mood, or how estrogen loss affects menopause, you’ll find real stories and real fixes—not just theory.
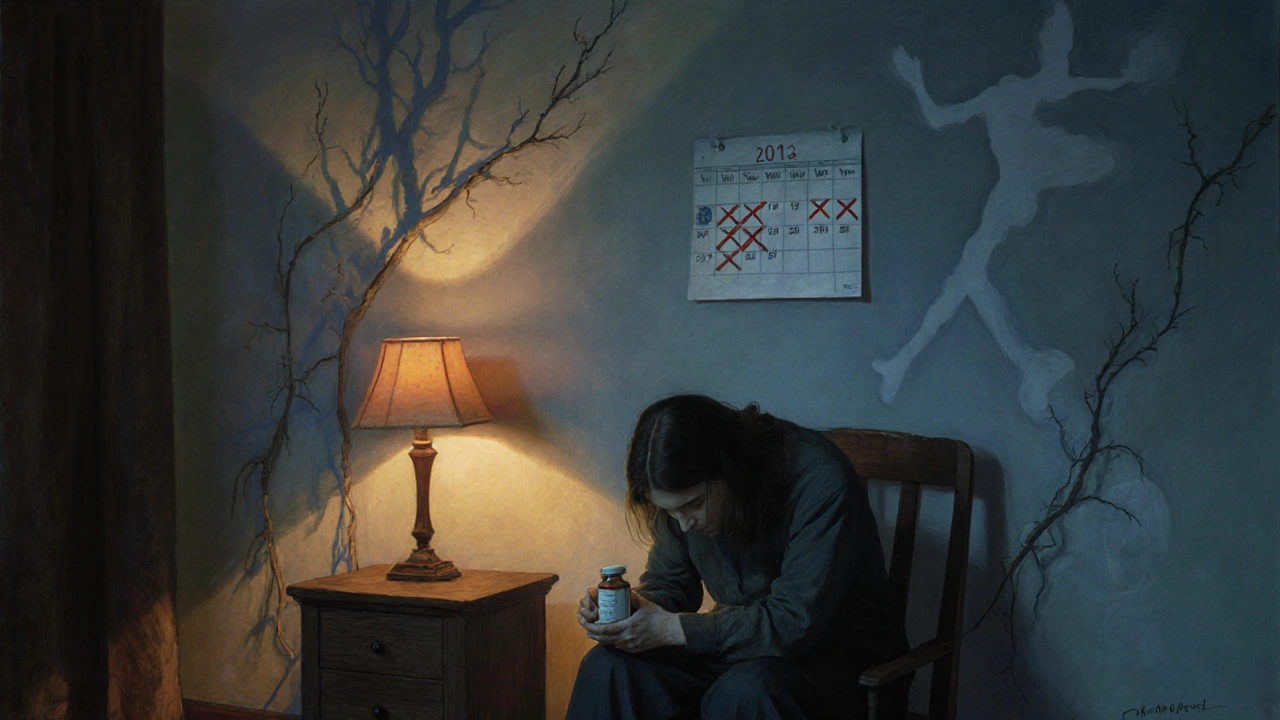
Long-Term Opioid Use: How It Affects Hormones and Sexual Function
Long-term opioid use disrupts hormone levels in over half of users, leading to sexual dysfunction, low libido, and menstrual issues. Learn how opioids affect testosterone and estrogen, what to ask your doctor, and safer alternatives for chronic pain.
Read more