When you're living with chronic pain, opioids can feel like a lifeline. But what happens when that lifeline starts quietly breaking down your body from the inside? For many people on long-term opioid therapy, the most overlooked side effects aren’t nausea or constipation-they’re hormonal chaos and sexual dysfunction. These aren’t rare quirks. They’re predictable, well-documented, and happening to over half of men and a large portion of women taking opioids for more than 90 days.
How Opioids Break Your Hormone System
Opioids don’t just block pain signals. They also hijack your brain’s control center for hormones. The hypothalamus, pituitary, and gonads-collectively called the HPG axis-work together to keep testosterone, estrogen, and cortisol levels balanced. Opioids like oxycodone, morphine, and fentanyl shut down the signal from the hypothalamus that tells your body to produce these hormones.
It’s not a guess. A 2020 meta-analysis in the Journal of Clinical Endocrinology and Metabolism found that 63% of men on long-term opioids develop low testosterone, known as hypogonadism. That’s more than 2 out of 3. Testosterone levels can drop 30-50% within just 30 days of starting therapy. For women, the picture is more complex: estrogen levels often stay normal, but testosterone drops, and menstrual cycles go haywire. Up to 87% of premenopausal women on chronic opioids experience irregular periods, and nearly 1 in 5 stop having periods entirely.
Even low doses matter. Studies show hormone disruption can begin at doses as low as 60 morphine milligram equivalents (MME) per day-about two 30 mg oxycodone tablets. At 120 MME or higher, the drop in testosterone becomes almost universal.
Sexual Function Takes a Hard Hit
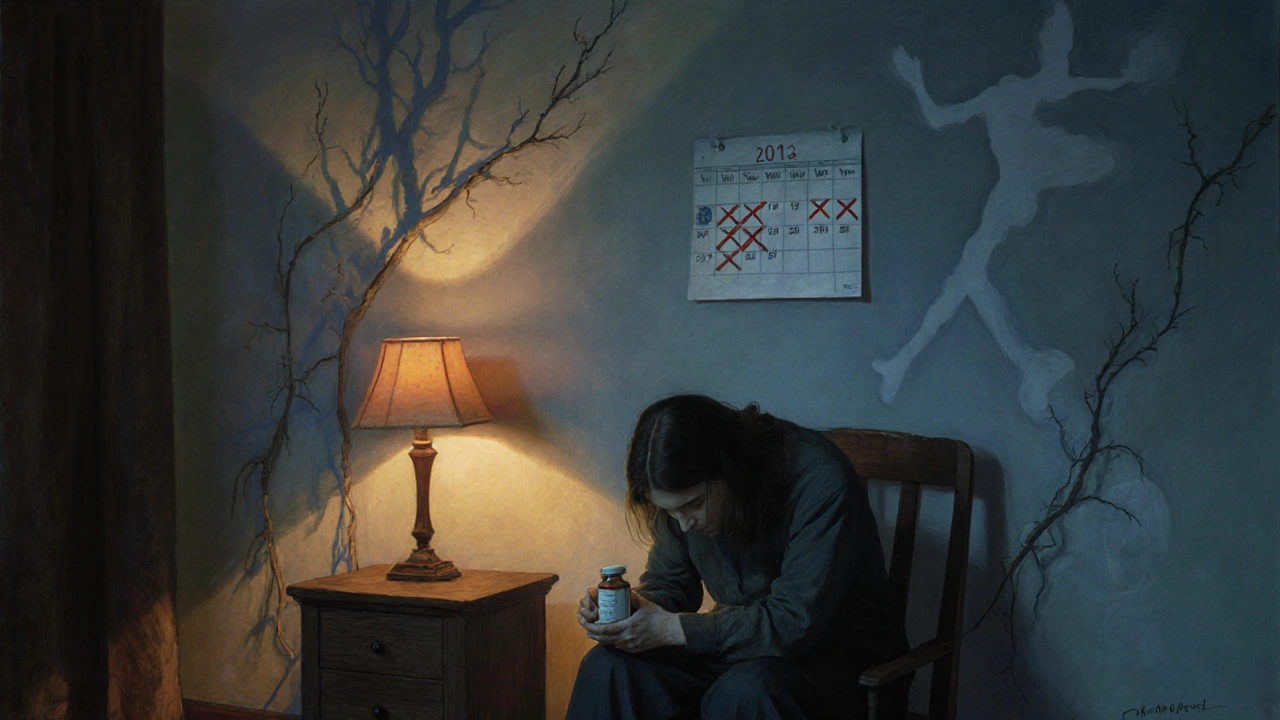
Low testosterone doesn’t just mean less muscle or energy. It directly kills libido, makes erections harder to get and keep, and reduces sexual satisfaction. Men on long-term opioids report decreased sex drive, erectile dysfunction, and even loss of morning erections. On Reddit’s r/ChronicPain community, one user wrote: “After two years on oxycodone, my testosterone hit 180 ng/dL. My doctor didn’t test it until I brought it up. Took six months to get help.”
Women aren’t spared. A 2021 survey of 342 women found 78% had lost interest in sex, 63% had irregular or absent periods, and 41% said their depression got worse. Many say their doctors dismissed these issues as “just part of chronic pain” or “aging.” But it’s not aging. It’s the opioids.
And it’s not just about sex. Hormonal imbalance affects mood, sleep, energy, and even bone density. Low testosterone is linked to increased fatigue, brain fog, and higher risk of osteoporosis. For women, low testosterone can contribute to vaginal dryness and pain during intercourse.
Opioids vs. Other Pain Treatments
Not all pain meds are created equal when it comes to hormones. Opioids are the worst offenders. Compare that to gabapentinoids like pregabalin-only 12% of men on these drugs show low testosterone. NSAIDs like ibuprofen or naproxen? Minimal to no effect on hormones. Even acetaminophen, while not perfect, doesn’t shut down your endocrine system the way opioids do.
That’s why guidelines from the American Pain Society and the CDC no longer recommend opioids as a first-line treatment for chronic non-cancer pain. They’re effective for acute pain-like after surgery or a broken bone-but for back pain, arthritis, or fibromyalgia? The risks outweigh the benefits. Studies show physical therapy, cognitive behavioral therapy, and certain antidepressants like duloxetine work better over time and don’t wreck your hormones.
What Doctors Should Be Doing (But Often Aren’t)
The Endocrine Society says it plainly: Every man on long-term opioids should get his testosterone checked before starting and every six months after. Women should be monitored for menstrual changes. Yet, a 2023 study found only 38% of primary care doctors routinely screen for this. Why? Because it’s not taught. Because it’s awkward. Because patients don’t bring it up.
Patients often feel embarrassed to talk about sex or libido changes. Doctors assume it’s depression or aging. But if you’re on opioids and your sex drive vanished, or your period stopped, it’s not in your head. It’s in your hormones.
And it’s fixable. Testosterone replacement therapy (TRT) helps 70-85% of men regain sexual function, energy, and mood when levels are restored. For women, off-label testosterone patches (1-2 mg daily) have shown promise in small studies, improving libido in about half of users. But TRT isn’t a magic bullet-it requires monitoring for side effects like increased red blood cell count, which can raise stroke risk.
What You Can Do Right Now
If you’re on opioids long-term and noticing changes in your sex life, energy, or menstrual cycle, here’s what to do:
- Ask for a blood test. Request total testosterone, free testosterone, LH, FSH, and cortisol. Don’t wait for your doctor to bring it up.
- Track your symptoms. Note changes in libido, erections, periods, mood, sleep, and energy. Bring this list to your appointment.
- Ask about alternatives. Is there a non-opioid option that could work? Could physical therapy, nerve blocks, or antidepressants help?
- Don’t quit cold turkey. Withdrawal can be brutal. If you want to reduce or stop opioids, work with a pain specialist. Unsupervised tapering leads to relapse in 73% of cases.
- Seek a multidisciplinary team. A pain doctor, endocrinologist, and therapist working together gives you the best shot at reclaiming your health.
New Hope on the Horizon
There’s progress. In 2023, the FDA approved Belbuca (buprenorphine buccal film), which causes 40% less hormone disruption than traditional opioids. Cleveland Clinic researchers found that combining low-dose naltrexone (a drug that blocks opioid receptors) with reduced opioid doses improved testosterone levels by 25-35% in two-thirds of patients-without losing pain control.
And the research is shifting. The NIH spent $15.7 million in 2024 on projects to reduce opioid side effects and develop better alternatives. By 2028, experts predict nearly half of pain clinics will routinely screen for hormone disruption. That’s up from just 12% in 2022.
But until then, the burden falls on you. If you’re on opioids and your body feels like it’s falling apart-your sex life gone, your energy gone, your mood off-don’t accept it as normal. Ask for help. Demand testing. Push for alternatives. You deserve more than just pain relief. You deserve to feel whole.
Do all opioids affect hormones the same way?
No, but most do. Morphine, oxycodone, and fentanyl are the strongest disruptors. Buprenorphine (especially in buccal form like Belbuca) causes significantly less hormone suppression-about 40% less than traditional opioids. Still, no opioid is completely safe for long-term hormone health.
Can I get my testosterone back if I stop opioids?
Often, yes. Many men see testosterone levels return to normal within 3-6 months after stopping opioids. But for some, especially those who used high doses for years, the damage may be longer-lasting. That’s why testosterone replacement therapy (TRT) is sometimes needed even after stopping opioids.
Why don’t doctors test for this more often?
Many doctors aren’t trained to look for it. Hormone disruption from opioids isn’t listed as a top side effect in most prescribing guides, and it’s uncomfortable to discuss. Patients often don’t bring it up either. But guidelines from the Endocrine Society and CDC clearly recommend screening. If your doctor won’t test you, ask for a referral to an endocrinologist.
Are women affected differently than men?
Yes. Men typically show low testosterone. Women often have normal estrogen but low testosterone, which affects libido and energy. The biggest red flag for women is menstrual disruption-missed periods, irregular cycles, or complete stoppage. These are not normal, even with chronic pain. Yet, research on female patients is extremely limited-only 2% of opioid trials include proper sexual function assessments.
Is testosterone replacement therapy safe?
For most men with confirmed low testosterone due to opioids, TRT is safe and effective when monitored. Risks include increased red blood cell count (polycythemia) in 15-20% of users, which can raise stroke risk. Regular blood tests every 3-6 months are required. TRT doesn’t cure pain, but it can restore energy, mood, and sexual function-making it easier to engage in other treatments like physical therapy.
What if I need opioids for severe pain?
For cancer pain, post-surgical recovery, or end-of-life care, opioids are still essential. The goal isn’t to avoid them entirely-it’s to manage the side effects. If you’re on opioids for legitimate reasons, ask your doctor to monitor your hormones and consider adding TRT or other support. You can have pain control and quality of life-it just takes a more thoughtful approach.

Malia Blom
November 3, 2025 AT 22:51So let me get this straight-we’re supposed to believe that opioids are this evil, hormone-destroying monster, but somehow NSAIDs are the saints of pain management? Please. I’ve been on ibuprofen for 12 years and my kidneys are screaming louder than my back. You’re trading one kind of destruction for another. Nothing’s clean. Nothing’s safe. Just because your testosterone drops doesn’t mean the pain magically disappears. Wake up.
Erika Puhan
November 4, 2025 AT 04:07The literature is unequivocal: chronic opioid exposure induces HPG axis suppression via μ-opioid receptor agonism at the hypothalamic level, resulting in diminished GnRH pulsatility, which subsequently reduces LH/FSH secretion and gonadal steroidogenesis. The data is robust, reproducible, and clinically significant. Yet, we continue to treat this as a lifestyle issue rather than a neuroendocrine pathology. This is not just negligence-it’s systemic epistemic failure.
Edward Weaver
November 5, 2025 AT 00:44Y’all are acting like this is some new discovery. We’ve known this since the 90s. The problem isn’t opioids-it’s that Americans want a magic pill for everything. You want energy? Go lift. You want sex drive? Get off the couch. You want your period back? Stop being a medical zombie. We’ve got a nation of people who think taking a pill is the same as living. This isn’t science-it’s entitlement.
Lexi Brinkley
November 5, 2025 AT 02:40THIS. SO. MUCH. 🙋♀️😭 I was on 120mg oxycodone for 3 years… lost my period, zero libido, felt like a ghost. My doctor said ‘it’s just stress.’ I cried in the parking lot. Then I found a pain clinic that actually listened. TRT changed my life. I’m not ‘fixed’… but I’m back. You’re not broken. You’re just medicated wrong. 💪❤️
Kelsey Veg
November 6, 2025 AT 17:37ok so like… i was on opioids for like 4 years after my back surgery and i just thought i was getting old? like my energy was gone and i didnt care about sex anymore and i was like ‘oh well, this is just what happens’… then i read this and i was like… wait. that’s not aging. that’s the drugs. i went to the doc and they were like ‘oh yeah we should’ve tested that’… i felt so stupid. but also like… why didn’t anyone tell me??
Alex Harrison
November 8, 2025 AT 03:19I’m a nurse and I see this all the time. Patients come in with low T and are shocked. They’ve been on opioids for years and no one ever checked. We’re trained to monitor for constipation and sedation, but not hormones. It’s not malice-it’s just not on the checklist. We need better protocols. And patients need to speak up. You’re not being dramatic if your sex life is gone. That’s a real side effect.
Jay Wallace
November 9, 2025 AT 08:35Let’s be real: if you’re on opioids long-term, you’re already choosing a compromised life. You want your hormones back? Then stop being lazy. You want your libido back? Then stop expecting a pill to fix your lack of discipline. The system is broken-but so are you. You think TRT is a solution? It’s a Band-Aid on a bullet wound. The real answer is: stop relying on opioids. Period.
Alyssa Fisher
November 10, 2025 AT 06:19What’s interesting here is how we’ve normalized suffering. We’ve turned chronic pain into a moral test: ‘if you’re not suffering, you’re not trying hard enough.’ But what if the suffering isn’t the pain-it’s the system that refuses to see you as a whole person? Hormones aren’t just chemistry-they’re identity. Libido isn’t a luxury. Energy isn’t a perk. When opioids steal those, they steal your sense of self. And no one talks about that. We talk about T levels, but not about the grief of losing the person you used to be.
Alyssa Salazar
November 11, 2025 AT 10:05Let me drop some jargon for a sec: the HPG axis suppression is dose-dependent and reversible in most cases-but only if you catch it early. The real tragedy isn’t the hormone drop-it’s the delayed diagnosis. Most patients are told it’s depression, aging, or ‘just chronic pain.’ But if you’re on >60 MME and your libido’s gone? That’s not ‘normal.’ That’s pharmacological iatrogenesis. And we’re not even tracking it properly in clinical trials. Especially for women. We need more gender-specific data.
Beth Banham
November 12, 2025 AT 08:52I’ve been on opioids for 8 years. I didn’t realize how much I’d lost until I started physical therapy and my energy came back-even without increasing my dose. I didn’t need to quit. I just needed to add something. It’s not all or nothing. You can have pain control and still feel human. I’m not yelling. I’m just saying… there’s hope. And you’re not alone.
Brierly Davis
November 12, 2025 AT 18:24You’re not weak for needing opioids. You’re not broken for losing your libido. You’re just caught in a system that treats pain like a math problem instead of a human experience. I’ve been there. I’ve cried in my car after a doctor told me ‘it’s all in your head.’ But here’s what I learned: ask for the test. Bring your symptom list. Find a doctor who listens. You deserve to feel whole again. I’m rooting for you. 💪❤️
Jim Oliver
November 13, 2025 AT 15:01Oh wow. A 1500-word essay on how opioids make you impotent. Groundbreaking. Next up: ‘Water causes dehydration.’ Shocking. You’re telling me the same thing the FDA said in 2016. Congrats. You win the Internet.
William Priest
November 15, 2025 AT 07:09Let’s not pretend this is some new revelation. This is basic endocrinology 101. The fact that primary care docs are still clueless speaks volumes about the state of American medicine. I’ve got a PhD in neuropharmacology and I still can’t believe how little we prioritize this. The real scandal isn’t the opioid crisis-it’s the silence around its biochemical consequences. You’re not being dramatic. You’re being ignored.
Ryan Masuga
November 15, 2025 AT 20:02my brother’s been on opioids for 6 years after his accident… he started TRT last year and his mood’s better, he’s sleeping better, he even started working out again. he still takes the meds, but now he’s got his life back. it’s not about quitting. it’s about adding the right support. don’t give up. talk to someone who gets it.
Jennifer Bedrosian
November 17, 2025 AT 01:11