Generic Medication Failure: Why Some Pills Don’t Work and What to Do
When a generic medication, a lower-cost version of a brand-name drug with the same active ingredient. Also known as therapeutic equivalent, it is approved by the FDA to work just like the original stops working for you, it’s not just in your head. For most people, generics work perfectly—saving up to 85% on costs without sacrificing results. But for some, even small differences in fillers, coatings, or manufacturing can cause real problems. This is what we call generic medication failure: when a patient notices a drop in effectiveness, new side effects, or a return of symptoms after switching from brand to generic.
This isn’t about poor quality. FDA rules require generics to have the same active ingredient, strength, and route of delivery. But they don’t require identical inactive ingredients—those are the binders, dyes, and preservatives that hold the pill together. For someone with a sensitive digestive system, a change in filler might slow absorption. For someone with epilepsy or asthma, even a 5% shift in how fast the drug enters the bloodstream can trigger seizures or breathing trouble. That’s why medication switching, the process of changing from one version of a drug to another, often for cost reasons needs to be handled carefully, especially with drugs that have a narrow therapeutic window. Think of blood thinners, thyroid meds, or anti-seizure pills. These aren’t like ibuprofen. A tiny change can mean the difference between control and crisis.
And it’s not just about the pill itself. therapeutic equivalence, the official term meaning two drugs produce the same clinical effect and safety profile doesn’t always match real-world experience. One study found that patients on generics for depression reported more side effects after switching—not because the drug changed, but because their brain had adapted to the exact formulation they’d been on for years. The same goes for transplant patients, where even a slight dip in drug levels can lead to organ rejection. If you’ve been stable on a brand-name drug for months or years, switching to generic isn’t always a simple swap. It’s a medical decision.
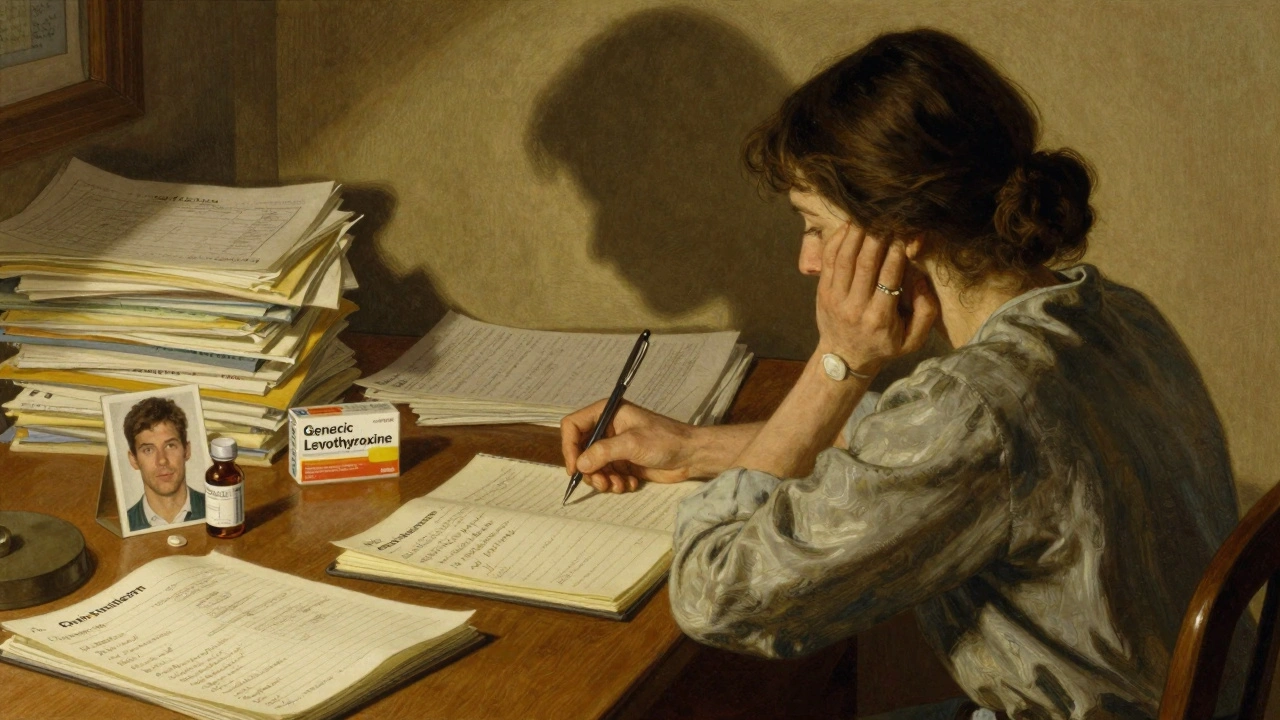
So what do you do if your generic isn’t working? First, don’t stop taking it. Track your symptoms: when did they start? Did they match the switch date? Write down how you feel—energy, mood, pain levels, sleep. Bring that to your doctor. Ask if your drug is on the list of those where switching is riskier. Ask about authorized generics, the exact same drug as the brand, made by the same company, just sold under a different name. They’re often cheaper than the brand and identical in every way. And if your insurer forces a switch, know your rights—many states allow exceptions for patients with documented issues.
The truth is, most people never have a problem with generics. But for the ones who do, the consequences can be serious. That’s why awareness matters. You’re not being difficult if your body reacts differently. You’re just one of the many who need personalized care—not just a price tag. Below, you’ll find real stories and expert advice on how to spot trouble early, talk to your doctor, and make sure your medication does what it’s supposed to—without putting your health at risk.
Insurance Appeals: Fighting Denials When a Generic Medication Doesn't Work
When generic medications fail, insurance often denies coverage. Learn how to fight back with proven steps, real examples, and free resources to get your brand-name drug approved.
Read more