Empagliflozin: What It Is, How It Works, and What You Need to Know
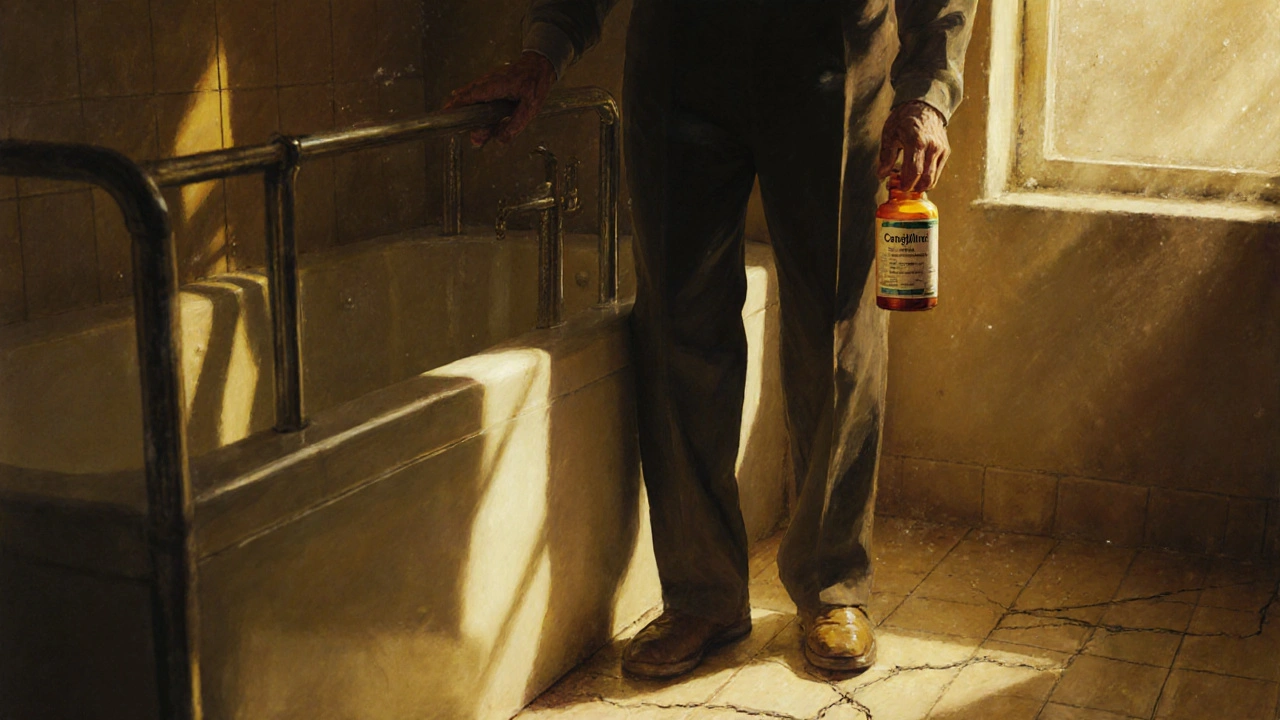
When you’re managing empagliflozin, a type of SGLT2 inhibitor used to treat type 2 diabetes by helping the kidneys remove excess sugar through urine. Also known as Jardiance, it’s not just another pill—it’s a medication that does something few others do: it lowers blood sugar while also cutting your risk of heart failure and kidney damage. This isn’t theoretical. Real-world studies show people taking empagliflozin are less likely to end up in the hospital for heart problems, even if they’ve already had a heart attack.
Empagliflozin works by blocking a protein in your kidneys called SGLT2. Normally, your kidneys reabsorb sugar back into your blood. Empagliflozin stops that, so sugar leaves your body through urine instead. That’s why you might notice more frequent urination—it’s the drug doing its job. Unlike insulin or metformin, it doesn’t make your pancreas work harder or cause low blood sugar on its own. It’s also linked to modest weight loss because you’re literally peeling off extra calories in the form of sugar. Many people start taking it because their doctor says their blood sugar isn’t under control, but they stick with it because they feel better—less bloating, more energy, and fewer heart-related scares.
It’s not for everyone. If you have severe kidney disease, it won’t work well. If you’re dehydrated or on diuretics, your doctor will check your fluid levels first. It’s also not a quick fix—you won’t see results overnight. But over weeks and months, the benefits add up: lower A1C, better blood pressure, and less strain on your heart. People with existing heart disease or chronic kidney disease often see the biggest gains. And unlike some older diabetes drugs, empagliflozin doesn’t cause weight gain—it often helps you lose a few pounds, which makes everything else easier.
It’s often paired with metformin, but it works fine on its own. You take it once a day, in the morning, with or without food. Side effects are usually mild—maybe a yeast infection or urinary tract infection, since sugar in your urine can feed bacteria. Drinking plenty of water helps. You won’t need constant blood tests like you do with some other drugs. But your doctor will still check your kidney function now and then.
What’s interesting is how empagliflozin fits into a bigger picture. It’s part of a newer class of diabetes drugs that treat more than just sugar. They protect your heart, your kidneys, and even your overall survival. That’s why it’s showing up in guidelines not just for diabetes, but for heart failure and kidney disease too—even if you don’t have diabetes. If you’re on it, you’re not just managing a number—you’re protecting your body in ways most pills can’t.
Below, you’ll find real stories and practical advice from people who’ve taken empagliflozin, what side effects they faced, how it changed their daily life, and how it compares to other drugs like dapagliflozin or canagliflozin. You’ll also see how diet, hydration, and exercise play into getting the most out of it. This isn’t just drug info—it’s life info.
SGLT2 Inhibitors and Bone Health: What You Need to Know About Fracture Risk
SGLT2 inhibitors help manage diabetes and protect the heart and kidneys, but canagliflozin may increase fracture risk in vulnerable patients. Empagliflozin and dapagliflozin appear safe for bone health.
Read more