SGLT2 Inhibitor Fracture Risk Calculator
Assess Your Fracture Risk
This tool helps you understand your fracture risk when taking SGLT2 inhibitors based on your specific medication and health factors.
When you're managing type 2 diabetes, choosing the right medication isn't just about lowering blood sugar. It's about balancing benefits with hidden risks - and one of the most confusing concerns lately is bone health. Specifically, could your SGLT2 inhibitor be making you more likely to break a bone? The answer isn't simple, and it depends heavily on which drug you're taking.
What Are SGLT2 Inhibitors?
SGLT2 inhibitors are a group of diabetes drugs that work differently from most others. Instead of pushing insulin out or making cells more sensitive to it, they tell your kidneys to dump extra sugar into your urine. That lowers blood glucose without causing low blood sugar or weight gain - two big wins. Common ones include canagliflozin (Invokana), empagliflozin (Jardiance), and dapagliflozin (Farxiga). They’re also known for protecting your heart and kidneys, which is why so many doctors prescribe them.
But in 2015, something unexpected popped up. The CANVAS trial, a major study on canagliflozin, showed more bone fractures in people taking it compared to those on placebo. That triggered a red flag from the FDA. Suddenly, patients and doctors were asking: Is this a one-drug problem? Or does it apply to all SGLT2 inhibitors?
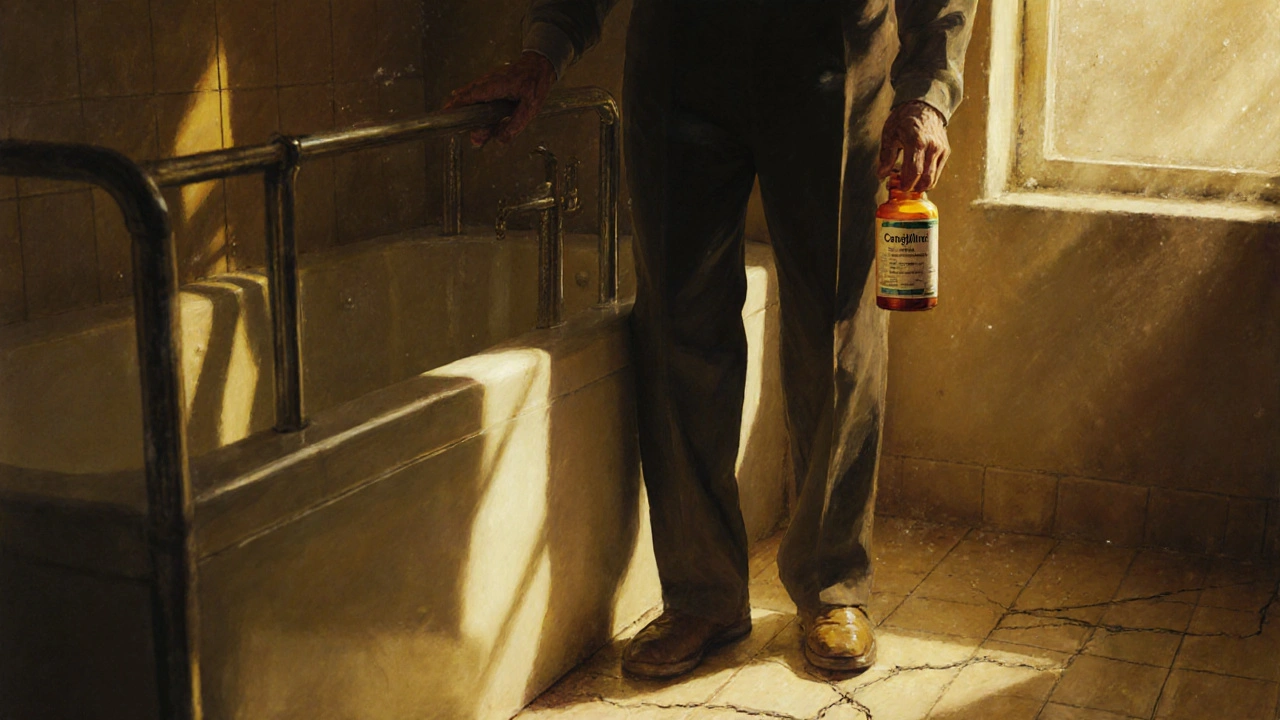
Canagliflozin and the Fracture Risk Signal
The data on canagliflozin is clear: it carries a higher fracture risk than other drugs in its class. In the CANVAS trial, people on canagliflozin had about 15 fractures per 1,000 patient-years, compared to 12 per 1,000 on placebo. That’s a 26% increase. The fractures weren’t from car crashes or sports injuries - they happened after simple falls, like stepping off a curb or slipping in the shower. Most occurred within the first 12 weeks of starting the drug.
Why? Three main theories exist. First, canagliflozin causes mild bone mineral density loss - about 1% at the hip and spine over two years, according to FDA-mandated studies. Second, it lowers estrogen levels slightly in women, which can weaken bone. Third, it can cause dizziness or low blood pressure when standing, increasing fall risk. These effects don’t happen with the same intensity in other SGLT2 inhibitors.
Here’s what’s important: the FDA only added a fracture warning to canagliflozin’s label - not to empagliflozin or dapagliflozin. That’s not an accident. It’s based on real data.
Other SGLT2 Inhibitors: Safer for Bones?
When you look at empagliflozin and dapagliflozin, the story changes. The EMPA-REG OUTCOME trial (2015) and DECLARE-TIMI 58 (2019) found no increased fracture risk with either drug. A 2023 meta-analysis of 27 clinical trials involving over 20,000 patients showed no overall link between SGLT2 inhibitors and fractures - except when canagliflozin was included. When researchers pulled canagliflozin out of the data, the risk vanished.
Real-world studies back this up. A 2023 analysis in the Journal of Parathyroid Disease reviewed patient records from over 50,000 people and found no connection between empagliflozin or dapagliflozin use and fractures. Even better: a 2023 study in JAMA Network Open showed that SGLT2 inhibitors overall had similar or even lower fracture rates than GLP-1 agonists and DPP-4 inhibitors - two other popular diabetes drug classes.
So if you're on empagliflozin or dapagliflozin, your fracture risk is likely no higher than if you weren’t taking any of these drugs at all.

Who’s at Highest Risk?
Not everyone on canagliflozin will break a bone. But some people are more vulnerable. The biggest risk factors include:
- Age over 65
- History of previous fractures
- Diagnosed osteoporosis (T-score ≤ -2.5)
- Low body weight or muscle mass
- History of falls or balance problems
- Long-term steroid use
Women, especially postmenopausal women, are more affected by the estrogen-lowering effect of canagliflozin. A clinical trial showed a 9.2% drop in estradiol levels after 24 weeks of 300 mg daily - enough to matter for bone health.
Dr. Sarah Chen, an endocrinologist at Mayo Clinic, says she avoids canagliflozin entirely in patients with osteoporosis or prior fractures. “I’ve seen three or four fractures per 1,000 patient-years with canagliflozin in elderly, high-risk patients,” she says. “That’s enough to change my prescribing habits.”
What Should You Do Before Starting?
If your doctor suggests an SGLT2 inhibitor, ask: Which one? And why?
For canagliflozin, the American Association of Clinical Endocrinologists (AACE) recommends checking your bone density with a DXA scan if you have any of the risk factors listed above. If your hip or spine T-score is below -2.0, they advise choosing another drug.
The American Diabetes Association’s 2023 guidelines now include a small adjustment to the FRAX fracture risk score - adding 0.5 points if you’re taking canagliflozin. No adjustment is made for empagliflozin or dapagliflozin. That’s a subtle but important distinction.
Here’s a quick checklist before starting any SGLT2 inhibitor:
- Do you have a history of fractures or osteoporosis?
- Are you over 65 or have balance issues?
- Are you on other medications that cause dizziness?
- Have you had a fall in the past year?
If you answered yes to any of these, talk to your doctor about switching to empagliflozin or dapagliflozin - unless there’s a strong reason not to.
Why the Confusion? The Data Is Messy
Why do some studies say there’s no risk, while others say there is? It comes down to how the data is grouped. Early studies lumped all SGLT2 inhibitors together. That masked the fact that canagliflozin was driving the risk. Later analyses that separated the drugs revealed the truth: the class isn’t the problem - one drug is.
Also, many trials were designed to study heart and kidney outcomes, not bones. They weren’t powered to detect small differences in fracture rates. Dr. Robert Heaney, a leading bone expert, points out that the number of fractures in these trials was too low to be statistically reliable. “We need longer follow-up,” he says. “We’re still missing part of the picture.”
But here’s what we know now: if you’re healthy and have no bone issues, any SGLT2 inhibitor is likely safe. If you’re at risk for fractures, avoid canagliflozin.

What About Other Diabetes Drugs?
It’s worth comparing SGLT2 inhibitors to other options. GLP-1 agonists like semaglutide (Ozempic) and liraglutide (Victoza) are popular, but they can cause nausea and vomiting - which increases fall risk in older adults. DPP-4 inhibitors like sitagliptin (Januvia) are neutral for bone health but offer less heart and kidney protection. Metformin? It’s safe for bones, but doesn’t protect the heart like SGLT2 inhibitors do.
For most people with diabetes and heart or kidney disease, the benefits of SGLT2 inhibitors outweigh the risks - as long as you pick the right one.
What’s Changing in 2025?
The field is evolving fast. The American Diabetes Association and European Association for the Study of Diabetes are preparing a new consensus report expected in early 2025. It will likely formalize the idea that canagliflozin should be avoided in high-risk bone patients - while other SGLT2 inhibitors remain first-line options.
Prescription trends already reflect this. Between 2017 and 2022, canagliflozin use dropped 22% in the U.S. Empagliflozin and dapagliflozin prescriptions rose by over 40%. The American Geriatrics Society’s 2023 Beers Criteria lists canagliflozin as “potentially inappropriate” for older adults with osteoporosis - but doesn’t mention the others.
Pharmacies and insurers are catching up too. Some now require pre-authorization for canagliflozin if you have a history of fractures.
Bottom Line: Know Your Drug, Know Your Risk
Don’t panic if you’re on an SGLT2 inhibitor. But do pay attention to which one.
If you’re on empagliflozin or dapagliflozin: your bone health is likely unaffected. Continue taking it - the heart and kidney benefits are real.
If you’re on canagliflozin and have osteoporosis, a past fracture, or are over 65 with balance issues: talk to your doctor about switching. The risk isn’t huge, but it’s real - and avoidable.
And if you’re just starting diabetes meds? Ask your doctor: “Which SGLT2 inhibitor are you recommending, and why?” Don’t assume they’re all the same. They’re not.
Do SGLT2 inhibitors cause bone loss?
Only canagliflozin has been consistently linked to small but measurable bone mineral density loss - about 1% over two years at the hip and spine. Empagliflozin and dapagliflozin show no significant effect on bone density in clinical trials.
Is it safe to take SGLT2 inhibitors if I have osteoporosis?
Avoid canagliflozin if you have osteoporosis or a prior fracture. Empagliflozin and dapagliflozin are considered safe alternatives. Always get a bone density scan (DXA) before starting canagliflozin if you have risk factors.
Why was canagliflozin singled out by the FDA but not the others?
Because the CANVAS trial showed a clear increase in fractures with canagliflozin - about 26% higher than placebo. Other major trials (EMPA-REG, DECLARE) found no such signal with empagliflozin or dapagliflozin. The FDA acts on drug-specific data, not class-wide assumptions.
Can SGLT2 inhibitors cause falls?
Yes, but indirectly. These drugs can cause low blood pressure when standing (postural hypotension), leading to dizziness and falls - especially in older adults. This risk exists with all SGLT2 inhibitors, but it’s more dangerous if you already have weak bones. Staying hydrated and rising slowly from sitting can help.
Should I get a bone density scan before starting an SGLT2 inhibitor?
If you’re over 65, have a history of fractures, or are diagnosed with osteoporosis, yes - especially if your doctor is considering canagliflozin. For empagliflozin or dapagliflozin, routine scanning isn’t needed unless you have other risk factors.
Are there any alternatives to SGLT2 inhibitors if I’m worried about bones?
Yes. Metformin is the safest for bone health and is still first-line for most people. GLP-1 agonists like semaglutide offer strong heart and weight benefits but may increase fall risk due to nausea. DPP-4 inhibitors are neutral for bones but offer less cardiovascular protection. Your doctor can help weigh the trade-offs.

Dana Dolan
November 19, 2025 AT 19:27So canagliflozin is basically the sketchy cousin of the SGLT2 family? 😅 I’m on Jardiance and just read this and thought I’d check-glad I’m not the one with the bone warning label. Still, weird how one drug in the class messes with bones but the others don’t. Like, why even make the whole class look bad because of one bad apple?
Frank Dahlmeyer
November 21, 2025 AT 08:26Let me tell you something-this is exactly why I stopped trusting pharmaceutical companies to just say ‘this drug is safe’ without breaking it down. They slap a whole class label on everything, and then you’ve got people like me, who’ve been on dapagliflozin for three years, suddenly getting scared because someone else’s prescription came with a fracture warning. But here’s the kicker: the data doesn’t lie. When you separate canagliflozin from the rest, the fracture risk disappears. That’s not a coincidence, that’s a pattern. And honestly, if your doctor prescribes you canagliflozin without asking about your fall history or bone density, you need a new doctor. Period. The FDA didn’t just pull that warning out of thin air-it was based on real numbers, real trials, real people breaking bones after stepping off a curb. This isn’t fearmongering, it’s medicine.
Timothy Reed
November 22, 2025 AT 11:02Thank you for this well-structured and evidence-based breakdown. As a primary care provider, I’ve started asking patients specifically which SGLT2 inhibitor they’re on before prescribing, and I now routinely screen for fracture risk factors before even considering canagliflozin. The distinction between the drugs is clinically meaningful, and I appreciate how the guidelines are catching up. For patients with osteoporosis or T-scores below -2.0, I now default to empagliflozin or dapagliflozin unless there’s a compelling reason not to. The heart and kidney benefits remain intact without the added bone risk. This is precision medicine at its best.
Christopher K
November 23, 2025 AT 06:50Oh wow, so now we’re policing diabetes meds based on who broke their hip after tripping over their dog? 🤡 Next they’ll ban metformin because someone fell off a ladder while trying to take their pills. This is why America’s healthcare system is a joke. You want to live longer? Take the drug. You want to avoid a fracture? Don’t trip. Stop treating adults like toddlers who need a warning label on their coffee. Canagliflozin isn’t dangerous-it’s just not for people who can’t walk straight. Maybe we should start requiring balance tests before giving out insulin too.
harenee hanapi
November 24, 2025 AT 09:14OMG I KNEW IT. I’ve been saying this for years. My aunt was on Invokana and then she fell in the shower and broke her hip-AND NO ONE LISTENED. They just said ‘oh it’s just a coincidence.’ But it wasn’t! It was the drug! And now you’re saying it’s true? I’m crying. I’ve been so lonely in this. Everyone thought I was being dramatic. But I knew. I just knew. And now the science agrees with me. Thank you for validating my pain. 🥺💔
Christopher Robinson
November 25, 2025 AT 06:25Big thanks for this! 🙏 I’m on Farxiga and have osteopenia (T-score -1.8), so this was super reassuring. I asked my endo about it last month and she said ‘no data for dapagliflozin’-so I’m glad to see the meta-analysis backs that up. Also, hydration tip: I drink 3L of water a day and rise slow from chairs. No dizziness. No falls. Just good vibes. 🌊🪑
James Ó Nuanáin
November 25, 2025 AT 15:10It is, of course, a matter of profound regret that the American regulatory apparatus has permitted such a disparity in drug safety profiles to persist for so long. The CANVAS trial, conducted with commendable rigour, demonstrated unequivocally that canagliflozin carries a statistically significant elevation in fracture incidence-a finding that ought to have been acted upon with alacrity. The fact that other SGLT2 inhibitors have been exonerated by subsequent analyses speaks not to their inherent safety, but rather to the necessity of disaggregating pharmacological data at the molecular level. One must not conflate mechanism with outcome. The kidneys may handle glucose similarly, but the systemic effects diverge markedly. This is not mere pharmacology-it is epistemology in action.
Nick Lesieur
November 26, 2025 AT 23:21So… you’re telling me the drug company didn’t test all these drugs the same way? Lmao. Of course they didn’t. Canagliflozin was the first one out the door-so they rushed the bone safety stuff. Then when the FDA said ‘uhhh this looks bad,’ they just slapped a warning on it and moved on. Meanwhile, Jardiance and Farxiga got to chill and look innocent because they came later and got lucky with trial design. Classic pharma. They don’t care about your bones-they care about patent expiry dates. 🤷♂️
Angela Gutschwager
November 28, 2025 AT 02:56Canagliflozin = bad. Others = fine. Stop overcomplicating it.
Andy Feltus
November 29, 2025 AT 23:54It’s funny how we treat drugs like they’re all the same-like ‘SGLT2 inhibitor’ is a personality trait. But drugs aren’t people. They’re molecules with different side effects. Canagliflozin isn’t evil-it’s just got a quirk. Like how some people are great at parties but terrible at math. The real question isn’t ‘should I take it?’ It’s ‘do I fit the profile where this quirk becomes a problem?’ If you’re 70, have osteoporosis, and your balance is questionable? Yeah, swap it. If you’re 50, active, and your bones are solid? Go ahead. The drug isn’t the villain. The blanket assumption is.
Dion Hetemi
November 30, 2025 AT 10:59Here’s the real problem: nobody’s talking about the fact that the fracture risk is highest in the first 12 weeks. That’s when you’re adjusting to the diuresis, the BP drop, the dehydration. So why aren’t we telling people to get a baseline bone scan *before* starting, and then another one at 3 months? Why are we just waiting for the hip to break? This is reactive medicine, not proactive. And it’s lazy. The data’s there-we’re just choosing not to act on it until someone’s in a cast. That’s not medicine. That’s gambling with people’s mobility.
Kara Binning
December 2, 2025 AT 04:47So let me get this straight-my doctor prescribed me Invokana because ‘it’s the most effective’ and now I’m supposed to feel guilty for having a hip fracture? I didn’t ask for this. I trusted my doctor. And now I’m being told I should’ve known to check my bone density? How? I’m not a doctor. I’m just a woman trying to survive diabetes. This is why I hate the medical system. You give us drugs like they’re candy, then blame us when they backfire. 🙄
Zac Gray
December 3, 2025 AT 19:11Good summary. I’ve been on Jardiance for 4 years-no falls, no fractures, great kidney numbers. My doctor switched me from canagliflozin after the 2017 FDA alert, and I’ve never looked back. The key takeaway? It’s not about avoiding SGLT2 inhibitors-it’s about choosing the right one. And if you’re over 65 or have a history of falls? Don’t gamble. Swap it. It’s not hard. Ask for the data. Ask for the scan. Your bones will thank you.
Steve and Charlie Maidment
December 5, 2025 AT 12:53Okay but let’s be real-why is it always the same group of people who get hurt? Elderly, osteoporotic, low weight, fall-prone. Why do we keep treating them like they’re disposable? We have the data. We know who’s at risk. So why aren’t we mandating bone scans before prescribing canagliflozin to anyone over 60? Why are we still letting insurance companies decide who gets screened? This isn’t about the drug-it’s about who gets protected and who gets left behind. And that’s the real tragedy here.
Michael Petesch
December 7, 2025 AT 09:07As someone from a country where diabetes care is under-resourced, I find this level of nuance refreshing. In many places, patients are simply given ‘a diabetes pill’ without any discussion of subtypes or risk profiles. The distinction between canagliflozin and the others is not just clinically important-it’s ethically imperative. To treat all SGLT2 inhibitors as interchangeable is to deny patients their right to informed choice. This post should be required reading for every medical student and primary care provider, especially in low-resource settings where follow-up is limited and consequences are permanent.