Doctor Communication: How to Talk to Your Doctor About Medications and Side Effects
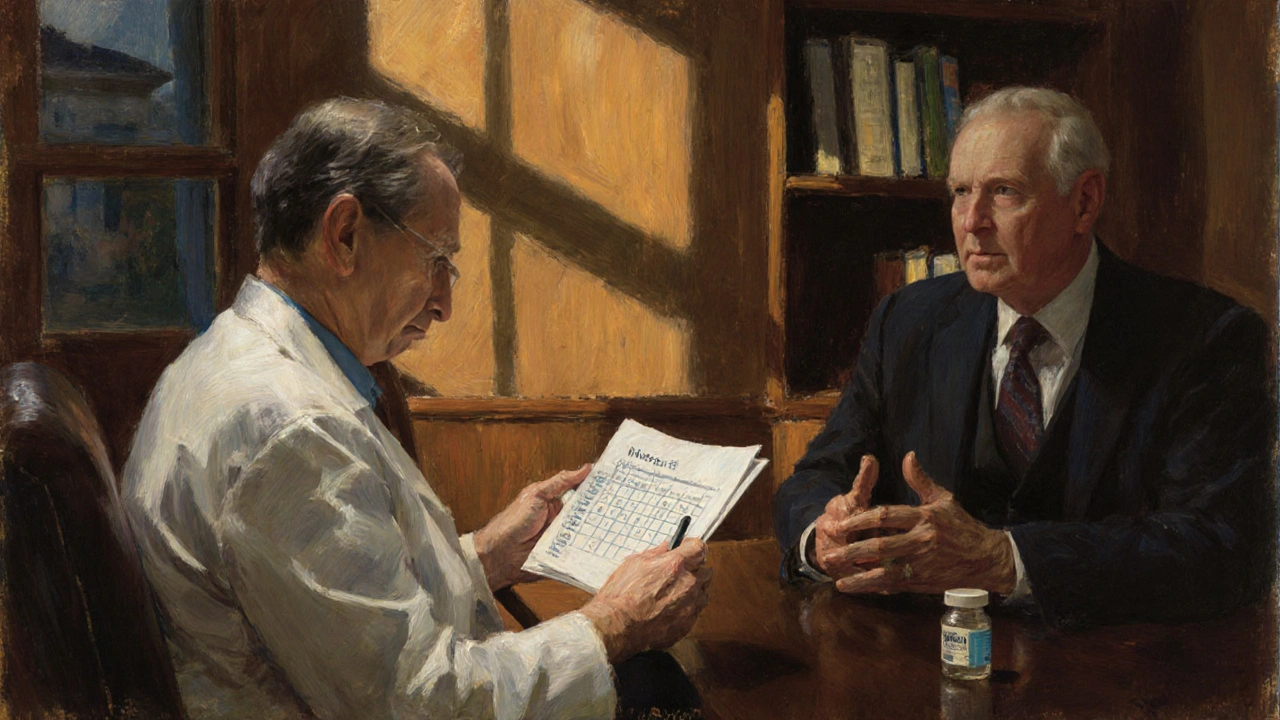
When it comes to your health, doctor communication, the clear, two-way exchange between patients and healthcare providers about treatment, symptoms, and concerns. Also known as patient-provider dialogue, it’s not just polite—it’s life-saving. Too many people leave the office with a prescription in hand but still confused about what they’re taking, why, or what could go wrong. You don’t need to be a medical expert to get the answers you deserve. You just need to know what to ask.
Medication safety, the practice of using drugs correctly to avoid harm, errors, or dangerous interactions depends almost entirely on how well you and your doctor talk. A study from the Journal of Patient Safety found that over 70% of medication errors happen because of poor communication—not because the drug was wrong, but because the patient didn’t understand the instructions. That’s why reading labels matters, but so does asking: "What happens if I miss a dose?" or "Could this interact with my fish oil or Tylenol?"
And then there’s drug side effects, unexpected reactions to medications that can range from mild to life-threatening. Sweating from antidepressants? Weight gain from steroids? Memory fog after benzodiazepines? These aren’t normal. They’re signals. But if you don’t mention them, your doctor might assume you’re fine. You don’t have to wait until your next appointment to speak up. A quick call or message can prevent a hospital visit.
Many people think their doctor already knows what they’re feeling—but doctors don’t read minds. They rely on what you tell them. If you’re on azathioprine, they need to know if you’re feeling unusually tired. If you’re taking SGLT2 inhibitors for diabetes, they need to know if you’ve had a fall. If you’re switching to a generic version of your epilepsy drug, you need to tell them if your seizures changed. These aren’t small details. They’re critical data points.
And don’t let cost silence you. If your medication is too expensive, say so. There are authorized generics, compounding options, or even manufacturer coupons you might not know about. Your doctor isn’t just there to write scripts—they’re there to help you find workable solutions. The same goes for sleep aids, pain meds, or hormones. If something’s not working, or it’s making you feel worse, it’s not your fault. It’s a system problem—and you’re the one who can fix it by speaking up.
Good doctor communication isn’t about being loud. It’s about being clear, consistent, and prepared. Write down your questions before the appointment. Bring a list of everything you take—even vitamins. Say "I’m worried" instead of "I think it’s nothing." And if you don’t understand something, say "Can you explain that again?" No one will judge you. They’ll respect you more for it.
Below, you’ll find real stories and practical guides from people who’ve been there—parents switching their child’s asthma meds, seniors stopping dangerous sleep pills, diabetics managing bone risk, and others who learned how to turn quiet visits into powerful conversations. These aren’t theory pieces. They’re battle-tested tips from real patients who refused to stay silent.
How to Talk About Stopping or Tapering a Medication Safely with Your Doctor
Learn how to safely talk to your doctor about stopping or tapering a medication. Get clear steps, expert-backed tapering schedules, and communication tips to avoid withdrawal and stay in control of your health.
Read more