Psoriasis and Arthritis: How These Conditions Connect and What You Can Do
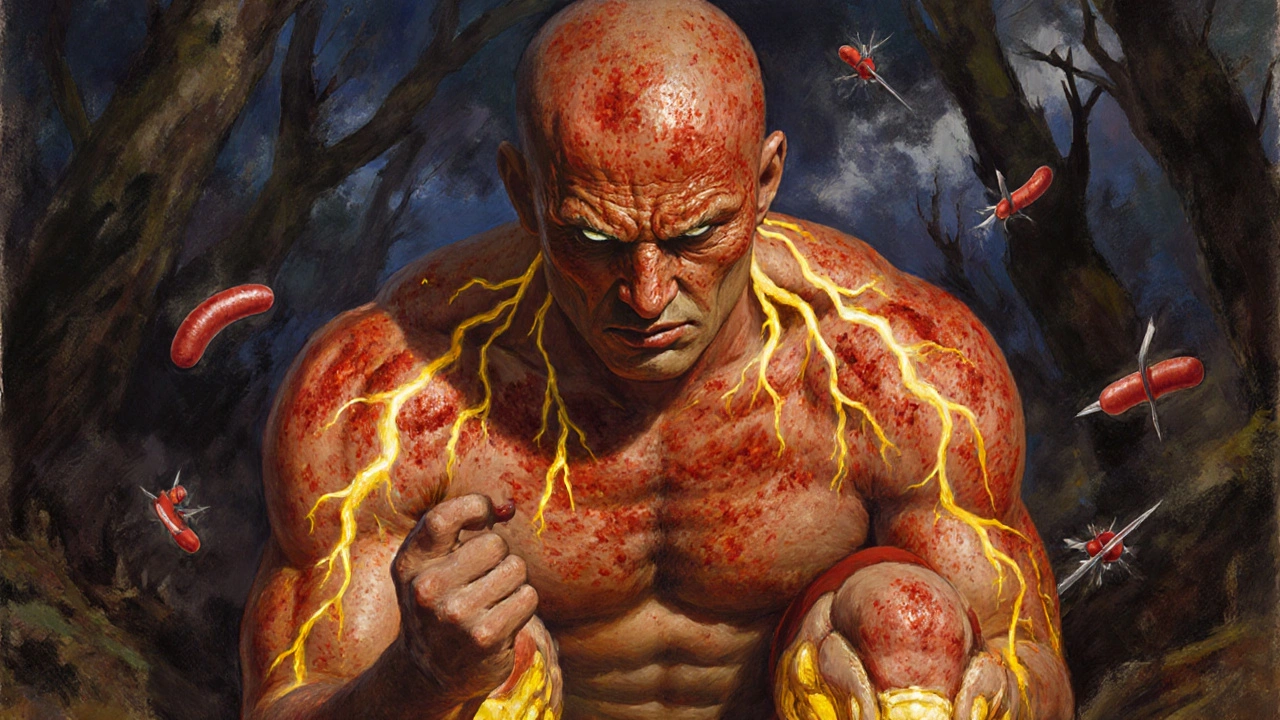
When you have psoriasis, a chronic skin condition that causes red, scaly patches due to overactive immune cells attacking healthy skin. Also known as plaque psoriasis, it doesn’t just affect how your skin looks—it can signal deeper problems in your body. Many people with psoriasis also develop psoriatic arthritis, a type of joint inflammation that comes with skin symptoms and can cause stiffness, swelling, and pain in fingers, toes, and larger joints. This isn’t random. It’s the same immune system going haywire, but this time targeting your joints instead of your skin. About 30% of people with psoriasis end up with joint issues, and it often shows up years after the skin first flares. If you’ve been dealing with dry, itchy patches and now your knuckles ache in the morning, this link matters.
What makes this tricky is that not all joint pain in psoriasis patients is psoriatic arthritis. Some people just get regular osteoarthritis from wear and tear, or rheumatoid arthritis from a different immune trigger. But if your joint pain matches your skin flare-ups—if your fingers swell like sausages or your lower back stiffens up after a bad psoriasis outbreak—you’re likely dealing with the real thing. The good news? Treatments that calm your immune system can help both your skin and your joints. Drugs like TNF blockers, IL-17 inhibitors, and even some oral meds used for psoriasis also reduce joint damage. Topical treatments like calcipotriol, a vitamin D-based cream that slows skin cell overgrowth and reduces redness. can manage flare-ups without affecting your joints, while systemic drugs tackle both. And yes, lifestyle matters too. Losing even 5% of body weight can cut inflammation enough to make a difference. Exercise keeps joints moving, and stress management helps because anxiety can trigger both skin and joint flares.
You’ll find real stories and practical tips in the posts below. Some cover how to spot early signs of joint involvement before it gets worse. Others break down which medications help both skin and joints, and which ones might make one worse. You’ll see how people manage daily life with stiff fingers and itchy elbows, how to talk to your doctor about testing, and what to do when your current treatment stops working. There’s no one-size-fits-all fix, but knowing how these two conditions connect gives you power—over your symptoms, your choices, and your future.
Psoriatic Arthritis: How Skin Disease Turns Into Joint Pain
Psoriatic arthritis links skin psoriasis with joint damage. Learn the warning signs, how it differs from other arthritis types, and why early treatment prevents permanent injury.
Read more