Pancreatic Cancer: A Practical Guide for Patients and Caregivers
Pancreatic cancer often hides until it’s advanced. That makes it scary, but knowing the common signs, the tests doctors use, and the realistic treatment options gives you more control. This guide is short, direct, and focused on what to do now if you or someone you love is facing this diagnosis.
Common signs and how it's diagnosed
Symptoms can be subtle: unexplained weight loss, upper belly pain that may move to the back, new or worsening diabetes, yellowing skin or eyes (jaundice), and loss of appetite. If you have persistent symptoms, push for a quick evaluation — early referral matters.
Doctors usually start with blood work and imaging. A contrast CT scan of the pancreas is the most common first test. MRI can help in some cases. Endoscopic ultrasound with a biopsy is often used to confirm the diagnosis. A blood marker called CA 19-9 may be checked, but it’s not a perfect test — it helps track disease in some patients, not screen for it.
Treatment choices and practical next steps
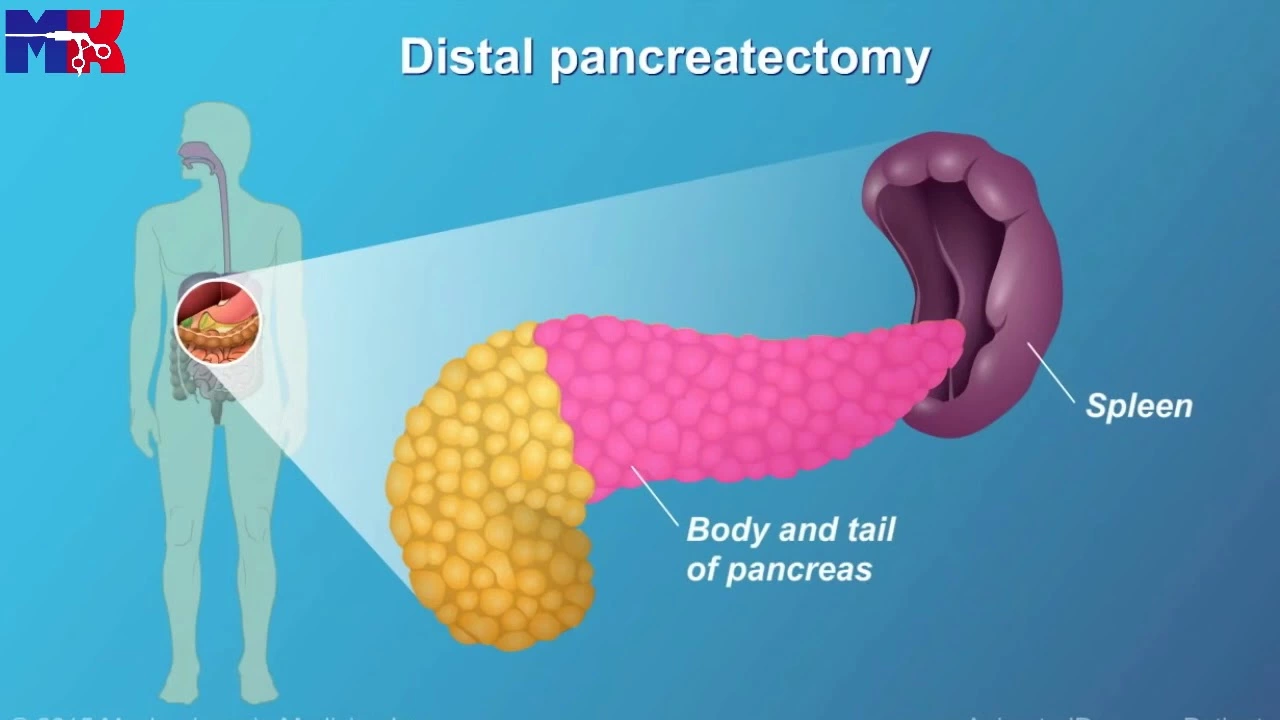
Treatment depends on where the tumor is and whether it has spread. If the cancer is caught early and is operable, surgery gives the best chance for longer survival — the Whipple procedure is common for tumors in the pancreas head. When surgery isn’t possible, chemotherapy is the main tool. Common regimens include FOLFIRINOX and gemcitabine with nab‑paclitaxel. For a small group with genetic changes like BRCA mutations, targeted drugs such as PARP inhibitors may help.
Radiation can be used in specific situations. Clinical trials are an important option — many new approaches combine chemotherapy with targeted therapy or immunotherapy. Ask your oncologist about trials at major centers or online registries.
Practical moves you can make right away: get a second opinion at a high-volume cancer center, ask for genetic testing (it can affect treatment choices), and connect with a dietitian early — maintaining weight and strength helps you tolerate treatment. Manage pain and blood sugar proactively; these issues are common and treatable.
Supportive care matters. Palliative care is not the same as giving up — it focuses on symptom control and quality of life and should start early, alongside cancer treatment. Social workers and patient groups can help with logistics, financial questions, and emotional support.
If you need medication or help finding affordable drugs, look for reputable pharmacy resources and talk to your care team about patient assistance programs. Keep records of scans and pathology reports — they make second opinions and trial applications faster.
Facing pancreatic cancer is hard, but clear steps — quick evaluation, accurate diagnosis, smart treatment choices, and strong symptom care — make a real difference. Use your team, ask for tests and opinions, and consider clinical trials when standard options are limited.
Pancreatic Cancer and Ethnicity: Understanding the Differences in Risk
As a blogger, I am compelled to shed light on the topic of pancreatic cancer and its varying risk factors, particularly in relation to ethnicity. It is essential to understand that different ethnic groups experience diverse levels of risk when it comes to this devastating disease. Research has shown that African Americans, for instance, have a higher incidence of pancreatic cancer compared to other ethnic groups. Additionally, genetic predispositions, environmental factors, and lifestyle choices play a significant role in determining one's risk for developing this form of cancer. By understanding these differences, we can work towards better prevention, early detection, and treatment methods tailored to individual needs.
Read more