Menstrual Migraines: What They Are and What Helps
Do your headaches show up around your period and hit harder than usual? Those could be menstrual migraines. They tend to start a day or two before bleeding and can last a few days. They’re often linked to the drop in estrogen that happens just before your period.
Menstrual migraines can feel different from other headaches. Expect throbbing pain on one side, light and sound sensitivity, nausea, and sometimes warning symptoms like visual changes. Because they follow a predictable schedule, you can often plan ahead instead of just reacting once the pain starts.
Quick ways to ease an attack
When a migraine hits, try to act fast. Rest in a dark, quiet room and use a cold pack on your forehead. Over-the-counter pain relievers like ibuprofen or naproxen can help if you can take them safely. Many people find these work best when started at the first sign of migraine, not after full pain sets in.
If OTC meds don’t cut it, prescription migraine-specific drugs called triptans often work quickly. These are best started early in the attack and should be used under your doctor’s guidance. Some people also get relief from anti-nausea meds or a short course of stronger painkillers, again only with medical advice.
Prevention and long-term control
Because menstrual migraines are predictable, short-term prevention can be very effective. Your doctor may suggest taking a preventive drug around the time your period starts—often a few days before and a few days into your period. Other options include continuous hormonal methods (like some birth control strategies) that reduce the hormonal swings that trigger attacks.
Daily magnesium supplements and keeping steady sleep, food, and caffeine routines can reduce frequency for some people. Tracking your cycle and symptoms in a simple app or diary helps spot patterns and makes it easier to discuss treatments with your healthcare provider.
Know when to see the doctor. If headaches are new, suddenly worse, come with fainting, confusion, fever, or visual loss, get medical help right away. Also talk to a clinician if your usual meds stop working or side effects become a problem. A clear treatment plan can make a big difference.
Small lifestyle changes add up: manage stress with short walks or breathing exercises, limit alcohol before your period, and aim for regular meals and sleep. These steps won’t stop every attack but can lower how often migraines happen and how bad they feel.
Menstrual migraines are common and treatable. Track your symptoms, try early treatment, and work with your doctor on a prevention plan that fits your life. You don’t have to just endure the pain—there are clear, practical ways to reduce it and take control of your cycle-related migraines.
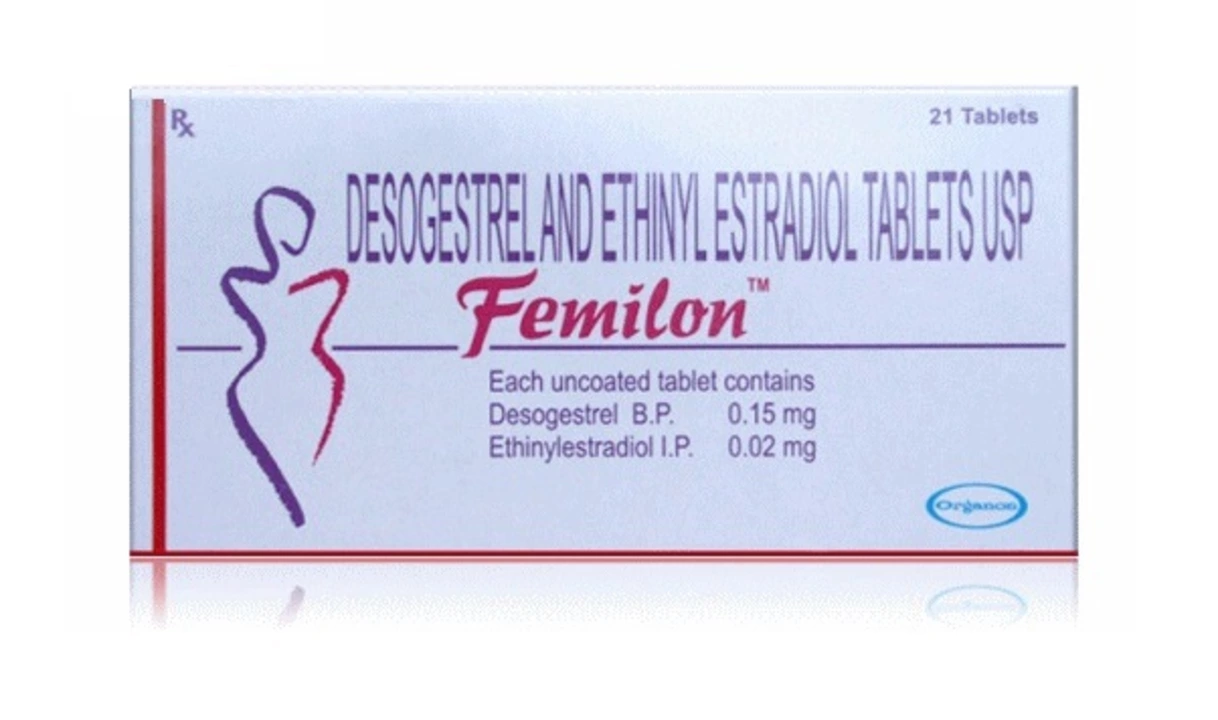
Ethinylestradiol and its Role in Managing Menstrual Migraines
As a sufferer of menstrual migraines, I've recently discovered the role of Ethinylestradiol in managing this painful condition. Ethinylestradiol is a synthetic estrogen hormone that can help stabilize hormonal fluctuations during the menstrual cycle. By doing so, it has the potential to reduce the frequency and severity of migraines associated with periods. Many women, including myself, have found relief by using birth control pills containing Ethinylestradiol. It's definitely worth discussing with your healthcare provider if you're struggling with menstrual migraines.
Read more