Donut Hole: What It Is and How It Affects Your Prescription Costs
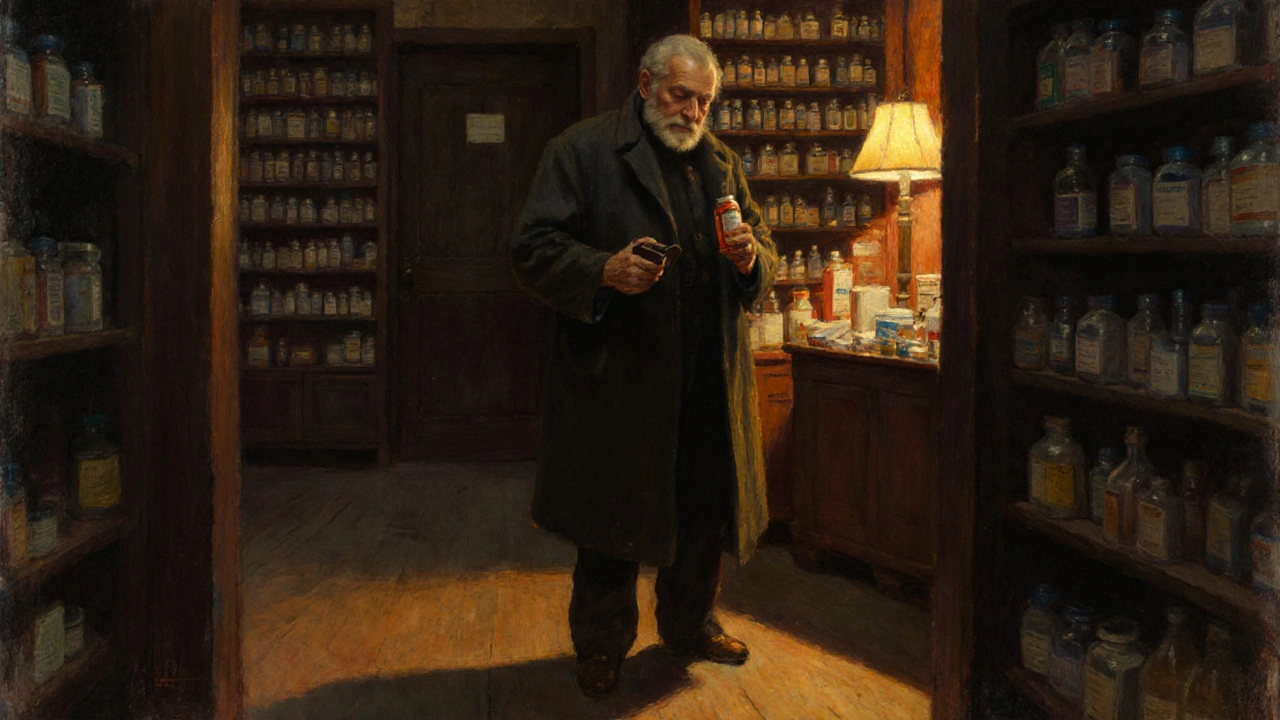
When you're on Medicare Part D, a federal program that helps cover the cost of prescription drugs for people on Medicare. Also known as prescription drug coverage, it’s meant to make meds affordable—but there’s a catch called the donut hole, a coverage gap where you pay more out-of-pocket after spending a certain amount on drugs.
The donut hole isn’t a glitch. It’s built into the system. Once you and your plan have spent a set amount on covered drugs in a year, you enter the gap. You’re still covered, but now you pay a bigger share—sometimes up to 25% or more—until you hit the catastrophic coverage threshold. This hits hardest for people taking multiple brand-name drugs or high-cost meds like insulin, cancer treatments, or autoimmune drugs. Many don’t realize they’re in the donut hole until their pharmacy says their copay just jumped from $10 to $50. It’s not a mistake. It’s the plan design.
What makes it worse is that the donut hole doesn’t disappear just because you switch to generics. Even if you’re on a cheaper version, your spending still counts toward the gap. But here’s the good part: since 2020, discounts on brand-name drugs in the donut hole have been phased in, and now you pay no more than 25% of the cost. That’s a big change from years ago when people paid 100%. Still, if you’re on expensive meds, that 25% can add up fast. That’s why knowing your plan’s specific thresholds matters. Some plans offer extra help during the gap. Some pharmacies have discount programs. And some people use authorized generics, the exact same drug as the brand name but sold under a different label at lower prices to stretch their budget. Others turn to compounding pharmacies, custom pharmacies that can make lower-cost versions of hard-to-find or overpriced drugs when the brand or generic isn’t affordable.
People in the donut hole aren’t alone. Over 3 million Medicare Part D enrollees hit it every year. And it’s not just about money—it’s about sticking with your treatment. Skipping doses because of cost leads to worse health, more ER visits, and higher bills down the road. That’s why understanding your plan’s structure, tracking your spending, and asking your pharmacist about alternatives is critical. You don’t have to suffer through the gap. There are ways to manage it. Below, you’ll find real guides on how to cut drug costs, spot hidden savings, and avoid surprises when your prescription price jumps. Whether you’re on insulin, antidepressants, or heart meds, these posts give you the tools to take control before the next bill arrives.
How to Manage Medication Costs During Medicare Part D Coverage Gaps (Donut Hole) in 2024-2025
Learn how to manage prescription drug costs during Medicare Part D’s coverage gap (donut hole) before it disappears in 2025. Save thousands with proven strategies, manufacturer discounts, and plan changes.
Read more