Imagine taking a pill that’s supposed to help you feel better-only to end up sicker. Nausea so bad you can’t eat, dizziness that makes you fall, or a rash that turns into a life-threatening reaction. This isn’t rare. About 6.7% of all hospital admissions in the U.S. are caused by bad reactions to medications. And for many, it’s not because they took too much. It’s because their body doesn’t process the drug the way doctors expect.
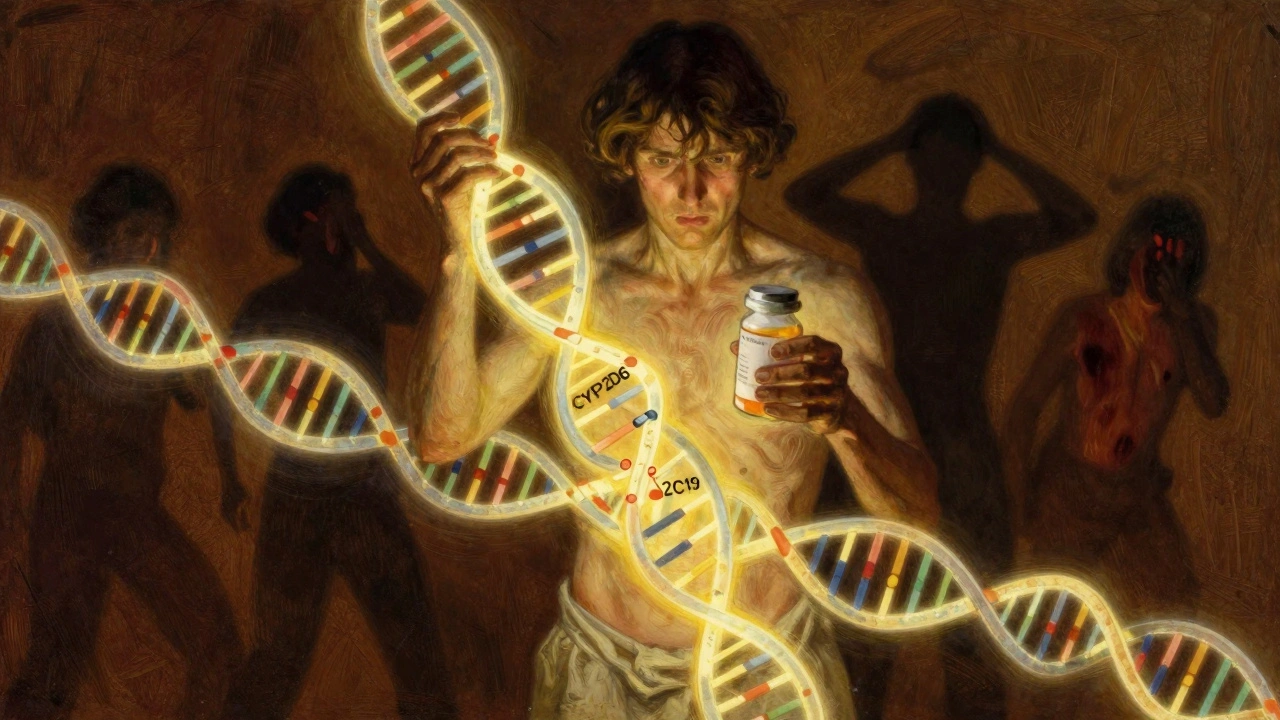
That’s where pharmacogenomics comes in. It’s not science fiction. It’s real, and it’s changing how medicine works. Pharmacogenomics studies how your genes affect the way you respond to drugs. Your DNA holds clues about whether a medication will work for you, whether it’ll cause side effects, or whether you need a higher or lower dose. This isn’t about guessing. It’s about using your genetic blueprint to pick the right drug, at the right dose, from the start.
How Your Genes Control How Drugs Work
Your body doesn’t treat every drug the same. It uses enzymes-mostly from the CYP family-to break down medications so they can be used or removed. But these enzymes don’t work the same in everyone. Some people have genes that make them ultra-fast metabolizers. Their bodies clear drugs too quickly, so the medication never has time to work. Others are slow metabolizers. Their bodies hold onto drugs too long, leading to dangerous buildup.
Take codeine, for example. It’s a common painkiller, but it doesn’t work unless your body converts it to morphine using the CYP2D6 enzyme. If you’re a poor metabolizer, codeine does nothing. If you’re an ultra-rapid metabolizer, you turn it into morphine too fast-and risk overdose, even at normal doses. There are real cases of babies dying after their breastfeeding mothers took codeine and passed too much morphine through breast milk. Genetic testing could have prevented that.
Same with clopidogrel, a blood thinner used after heart stents. About 30% of people have a variant in the CYP2C19 gene that makes the drug useless. These patients are at high risk of heart attack or stroke because the drug doesn’t work. But if you know ahead of time, doctors can switch you to a different medication like prasugrel or ticagrelor-no second heart attack needed.
What Gets Tested? The Key Genes and Drugs
Not every drug needs genetic testing. But for the ones that do, the science is solid. The Clinical Pharmacogenetics Implementation Consortium (CPIC), which sets global standards, has guidelines for 42 gene-drug pairs as of 2023. The most well-established include:
- CYP2D6 and antidepressants like fluoxetine, paroxetine, and codeine
- CYP2C19 and clopidogrel, citalopram, and proton pump inhibitors
- CYP2C9 and warfarin (blood thinner)
- HLA-B*15:02 and carbamazepine (for seizures)-carrying this gene increases the risk of a deadly skin reaction called SJS/TEN by 1,000 times
- HLA-B*57:01 and abacavir (for HIV)-testing is required before use because of the high risk of fatal allergic reaction
- TPMT and thiopurines (used in cancer and autoimmune diseases)-slow metabolizers can develop life-threatening bone marrow suppression
These aren’t theoretical. The FDA requires or recommends genetic testing for these drugs. For abacavir, testing is mandatory. For carbamazepine, it’s strongly advised for people of Asian descent. And for warfarin, dosing algorithms now include CYP2C9 and VKORC1 gene results to get the dose right on the first try.
Testing usually comes from a simple cheek swab or blood sample. Labs analyze around 25 genes that cover 70-80% of clinically important drug-gene interactions. The accuracy? Better than 99.5%. This isn’t a rough guess. It’s a precise readout.

Real Results: When Genetic Testing Changes Outcomes
Studies show this isn’t just theory-it saves lives and reduces suffering.
In psychiatry, a 2022 meta-analysis found that patients with major depression who got treatment guided by genetic testing had a 30.8% remission rate-compared to just 18.5% for those on standard care. That’s a 66% increase in people getting better. The number needed to treat? Just 8.2. Meaning, for every 8 people tested and switched to the right drug, one person avoids years of failed treatments.
One patient in Mayo Clinic’s program had tried 15 different antidepressants over 15 years with no success. Genetic testing revealed she was an ultra-rapid metabolizer of CYP2D6. Her body was breaking down paroxetine too fast. When her doctor switched her to bupropion-something her genes said would work-her depression lifted completely in eight weeks.
On Reddit, a user named MedStudent2023 shared how testing saved them from six months of constant nausea. They were on codeine for pain, but their CYP2D6 results showed they were a poor metabolizer. The drug wasn’t working, and the side effects were unbearable. Switching to tramadol eliminated the nausea and gave them real pain relief.
But it’s not perfect. In the TAILOR-PCI trial, which looked at over 1,200 heart patients, genotype-guided clopidogrel dosing didn’t show a statistically significant reduction in heart events compared to standard care. That surprised many. Why? Because earlier studies showed clear benefits. The answer may lie in how the trial was designed, or that newer drugs like ticagrelor were used more often in the control group. It’s a reminder: science evolves, and not every study gives a clear answer.
Why Isn’t Everyone Getting Tested?
If this works so well, why aren’t doctors ordering these tests for everyone?
First, the evidence isn’t there for all drugs. Right now, only about 15-20% of commonly prescribed medications have actionable genetic information. That means for most drugs-like your everyday antibiotics or blood pressure pills-genetics doesn’t change the decision.
Second, integration is hard. Only 37% of hospitals have successfully added pharmacogenomic results into their electronic health records. Even when results are available, many doctors don’t know how to use them. A 2022 survey found that 68% of pharmacists needed extra training to interpret results, especially for complex genes like CYP2D6, which has over 100 known variants.
Insurance coverage is another barrier. In the U.S., 89% of commercial plans cover PGx testing for cancer drugs-but only 47% cover it for psychiatric medications. That’s a huge gap. If you’re struggling with depression and your doctor wants to test you, you might have to pay out of pocket.
And there’s a data gap. Most genetic studies have been done in people of European ancestry. That means the guidelines may not apply as well to people of African, Asian, or Indigenous descent. The NIH’s All of Us program is trying to fix that by collecting genetic data from 3.5 million people-many from underrepresented groups. Results are expected in 2024, and they could change how we interpret results for millions.

Where Is This Headed?
The future is accelerating. The global pharmacogenomics market is projected to grow from $5.1 billion in 2022 to over $23 billion by 2030. The FDA is pushing for mandatory testing on 12 more drugs by 2025-including statins, SSRIs, and warfarin. PharmGKB predicts that by 2027, half of all commonly used medications will have genetic guidance.
And the tools are getting better. CPIC offers free online tools like the Guideline Viewer and PharmCAT to help doctors interpret results. Hospitals like the University of Florida have built full programs: 1,200 clinicians trained, 28 clinical alerts built into their EHR, and pharmacists on call to review every test result.
But the biggest shift? Moving from reactive to proactive. Instead of waiting for a bad reaction, some clinics are testing patients before they even get a prescription. Mayo Clinic has preemptively genotyped over 15,000 patients. Their idea: if you know your genes, you never have to guess again.
Should You Get Tested?
If you’ve had multiple medications fail, or if you’ve had a serious side effect you can’t explain, genetic testing could be life-changing. It’s especially worth considering if you’re starting:
- Antidepressants or antipsychotics
- Blood thinners like warfarin or clopidogrel
- Pain medications like codeine or tramadol
- Chemotherapy or immunotherapy drugs
- Drugs for epilepsy or autoimmune conditions
Ask your doctor if pharmacogenomic testing is right for you. You don’t need to be sick to benefit. If you’re on a long-term medication and it’s working fine, you may not need it. But if you’ve been through the trial-and-error cycle-trying drug after drug with no luck or too many side effects-this could be the key.
And if your doctor says, ‘We don’t do that here,’ ask why. Maybe they don’t have the tools. Maybe they’re not trained. But the science is there. And it’s getting harder to ignore.
Pharmacogenomics isn’t about replacing doctors. It’s about giving them better tools. It’s about turning guesswork into precision. It’s about making sure the next pill you take doesn’t hurt you-and actually helps.

nikki yamashita
December 12, 2025 AT 05:44Robert Webb
December 13, 2025 AT 06:32Stacy Foster
December 13, 2025 AT 12:50Ashley Skipp
December 15, 2025 AT 07:22wendy b
December 15, 2025 AT 10:54Audrey Crothers
December 16, 2025 AT 05:37Reshma Sinha
December 17, 2025 AT 00:47Lawrence Armstrong
December 17, 2025 AT 21:29Donna Anderson
December 18, 2025 AT 01:56Levi Cooper
December 19, 2025 AT 13:48sandeep sanigarapu
December 20, 2025 AT 09:10Nathan Fatal
December 20, 2025 AT 21:21Adam Everitt
December 20, 2025 AT 23:08Rob Purvis
December 22, 2025 AT 03:35Laura Weemering
December 22, 2025 AT 08:51