When someone says pancreatic cancer, most people think of a death sentence. And for a long time, that was true. But things are changing - slowly, but definitely. The truth is, if you catch it early, survival isn’t hopeless. The real problem? Most people don’t know the early signs until it’s too late. That’s why understanding the warning signals and what’s new in treatment matters more than ever.
The pancreas sits deep behind your stomach, making it hard to feel anything wrong. That’s one reason pancreatic cancer sneaks up on you. By the time symptoms show up, the cancer has often spread. But there are clues - real, measurable signs - that can point to trouble long before a tumor grows large enough to be seen on a scan.
What Are the Real Early Symptoms?
Forget the idea that pancreatic cancer only causes pain. That’s not the full story. In fact, the earliest signs are quiet, confusing, and easily mistaken for something else. Here’s what actually shows up before the disease becomes advanced:
- Unexplained weight loss - Losing 10 pounds or more without trying happens in about 60% of cases. It’s not just about eating less. Your body is changing how it uses energy.
- Jaundice - Yellow skin and eyes. This isn’t just a sign of liver trouble. When a tumor blocks the bile duct (common with head tumors), bilirubin builds up. Dark urine and pale, greasy stools often come with it. Itching is another hidden symptom - 60% of jaundiced patients feel it.
- New-onset diabetes - If you never had diabetes before, and suddenly your blood sugar spikes (over 126 mg/dL fasting), that’s a red flag. Research from Columbia University shows 80% of pancreatic cancer patients developed diabetes within 18 months of diagnosis. It’s not a coincidence - the tumor is messing with insulin production.
- Abdominal or back pain - This affects 65-75% of patients. The pain isn’t sharp. It’s a dull, constant ache that gets worse after eating or lying down. Many mistake it for gallstones or a pulled muscle.
- Loss of appetite and nausea - You’re not hungry. Even food you used to love feels disgusting. Nausea comes with it. These symptoms show up in over 45% of cases.
- Depression or anxiety - This one surprises people. A 2018 study found 33-45% of patients had major mood changes - sometimes as their first symptom - months before physical signs appeared. It’s not just stress. The cancer itself affects brain chemistry.
Most people see one or two of these symptoms and go to the doctor. But they get told it’s IBS, acid reflux, or aging. The average time from first symptom to diagnosis? Over four months. And by then, it’s often too late.
Why Is It So Hard to Diagnose Early?
The pancreas hides. It’s tucked behind your stomach, surrounded by organs. You can’t feel a tumor during a physical exam. Standard blood tests don’t catch it. Even a routine CT scan might miss tumors smaller than 2 cm.
Doctors rely on a few tools:
- CT scans - Good for tumors over 3 cm, but only 60% accurate for smaller ones.
- CA 19-9 blood test - Often elevated in advanced cancer, but misses early cases. Sensitivity? Just 30-50%.
- Endoscopic ultrasound (EUS) - A thin scope with a camera is inserted through the mouth into the digestive tract. It can grab tissue samples with 95% accuracy. This is the gold standard for confirming diagnosis.
There’s no screening test for the general public. That’s why experts focus on high-risk groups: people with inherited gene mutations (like BRCA2), a family history of pancreatic cancer, or chronic pancreatitis. For them, annual EUS or MRI scans starting at age 50 can catch tumors before they spread.
But here’s the breakthrough: new blood tests are coming. The PancreaSeq test from Johns Hopkins detects DNA from tumor cells in the blood. In high-risk people, it’s 95% accurate at spotting early cancer. Another test, being tested in the DETECTA trial, looks for protein markers and tumor DNA together - and it’s already hitting 85% accuracy in early trials.

What Are the Latest Treatment Advances?
Treatment has changed more in the last five years than in the last 50.
Surgery is still the only cure - but only if the cancer hasn’t spread. The Whipple procedure (removing the head of the pancreas, part of the small intestine, gallbladder, and bile duct) is still the go-to. At top centers like Memorial Sloan Kettering, patients with stage I cancer who get surgery have a 20-25% chance of surviving five years.
But now, surgery isn’t always the first step.
Neoadjuvant therapy - that’s chemo before surgery - is becoming standard. FOLFIRINOX (a mix of four drugs) shrinks tumors in 58% of borderline resectable cases. This means more people who once couldn’t have surgery now can. And those patients live longer.
For those with advanced cancer, survival has doubled since 2000. In 2022, the PRODIGE 24 trial showed patients on modified FOLFIRINOX lived a median of 54.4 months - nearly four and a half years - compared to 20.2 months with older chemo. That’s not a cure, but it’s life.
Targeted therapies are changing the game for specific subgroups:
- If you have a BRCA1 or BRCA2 gene mutation (about 5-10% of cases), olaparib can delay cancer growth for 7.4 months longer than placebo. It’s not a cure, but it gives time.
- If your tumor has MSI-H or dMMR (only 3-4% of cases), pembrolizumab - an immunotherapy - works in 40% of patients. That’s huge for a cancer that usually ignores immunotherapy.
And now, AI is helping. Google Health’s LYNA algorithm looked at 10,000 tissue slides and spotted pancreatic cancer with 99.3% accuracy. It doesn’t replace pathologists - it helps them find the tiniest signs they might miss.
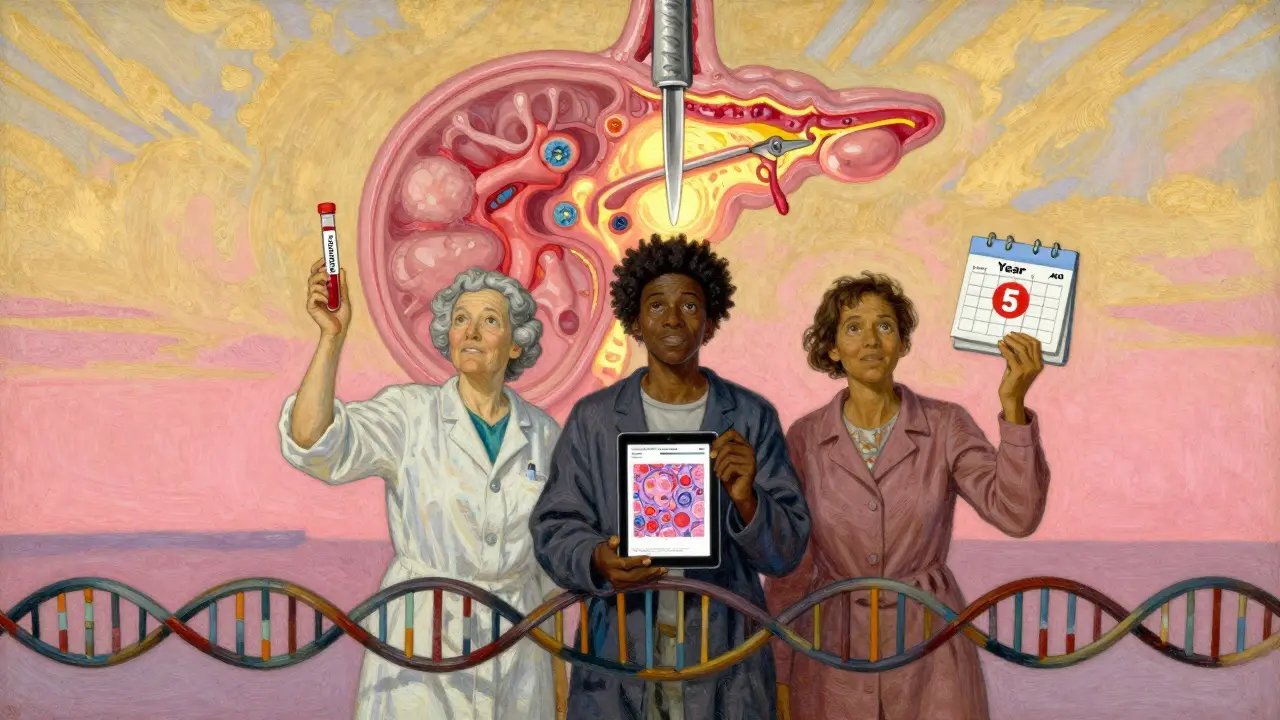
Who Should Be Screened?
Not everyone needs screening. But if you fit any of these, talk to your doctor:
- You have two or more close relatives with pancreatic cancer.
- You carry a BRCA1, BRCA2, PALB2, or Lynch syndrome mutation.
- You have hereditary pancreatitis.
- You’ve developed new-onset diabetes after age 50, especially if you’re not overweight.
- You have unexplained weight loss, jaundice, or persistent abdominal pain.
For these people, annual MRI or EUS scans can catch cancer early enough to remove it. And that’s the difference between a 3% survival rate and a 44% one.
What’s Next?
The future is multi-layered. Researchers aren’t just looking at one test - they’re combining blood markers, DNA fragments, protein changes, and even gut bacteria patterns. The ESPAC study is testing a combo of CA19-9, TIMP1, LRG1, and tumor DNA - and early results show 89% sensitivity.
One thing is clear: we’re moving away from “wait until it’s big” to “find it before it spreads.” The National Cancer Institute’s goal? Cut pancreatic cancer deaths by 25% by 2030. That’s ambitious. But with new tools, it’s possible.
And for patients? It means more time. More options. More hope.
Can pancreatic cancer be detected with a routine blood test?
No, a standard blood test like a CBC or metabolic panel won’t detect pancreatic cancer. The CA 19-9 test is sometimes used, but it’s not reliable for early stages - it misses up to half of early tumors. It’s more useful for monitoring treatment in known cases. New multi-marker blood tests are in trials and show promise, but they’re not yet standard.
Is pancreatic cancer hereditary?
About 10% of pancreatic cancers are linked to inherited gene mutations. The most common are BRCA1, BRCA2, PALB2, Lynch syndrome (MLH1, MSH2, MSH6, PMS2), and familial atypical multiple mole melanoma (FAMMM). If you have a strong family history - two or more close relatives with pancreatic cancer - genetic testing is recommended, even if you don’t have symptoms.
Why does pancreatic cancer cause new-onset diabetes?
Pancreatic cancer cells, especially in the head of the pancreas, can interfere with insulin-producing beta cells. This disrupts blood sugar control. In many cases, the cancer triggers insulin resistance or destroys these cells before it’s visible on a scan. That’s why sudden diabetes after age 50 - especially without risk factors like obesity - is a major red flag.
Can you survive pancreatic cancer if it’s caught early?
Yes. If the cancer is confined to the pancreas and hasn’t spread to blood vessels or lymph nodes, surgery can remove it. In that case, the five-year survival rate jumps to 44%. That’s why early detection matters. Only 12% of all cases are caught at this stage - but for those who are, survival is realistic.
What’s the most effective treatment for advanced pancreatic cancer?
Modified FOLFIRINOX is currently the most effective first-line chemo for advanced cases. It’s a four-drug combo that extends life by over two years compared to older treatments. For patients with BRCA mutations, adding olaparib after chemo can delay progression. Immunotherapy with pembrolizumab works only for the rare 3-4% with MSI-H tumors. Treatment is now personalized based on genetics and tumor biology.


Vamsi Krishna
February 13, 2026 AT 08:00Let me tell you something nobody else will: I had a cousin who lost 15 pounds in two months and got diagnosed with diabetes outta nowhere. Doctor said it was stress. Six months later, he was dead. Pancreatic cancer doesn’t care if you’re healthy. It doesn’t care if you eat kale. It just waits. And when it strikes? It’s silent. That’s why I’m screaming this into the void - if you’re losing weight for no reason, stop Googling ‘metabolism’ and get an EUS. Now. Not next month. Now.
Steve DESTIVELLE
February 14, 2026 AT 07:19The truth is we live in a world where medicine is more about profit than truth and the pancreas is just one more organ they let rot because it doesn’t make enough money to justify screening everyone but if you think about it deeply the real disease isn’t cancer it’s the system that waits until you’re dying to care and if you’re lucky you have insurance or a rich uncle or a doctor who actually listens but most people just get told to take antacids and wait for the next symptom to show up like pain or jaundice or depression or sudden diabetes all signs that were there months before they became visible on a scan
Stephon Devereux
February 15, 2026 AT 07:56This is one of the most important posts I’ve read all year. Seriously. The stats are terrifying but also empowering. We’ve been conditioned to think pancreatic cancer = death sentence. But look - 44% five-year survival when caught early? That’s not just hope, that’s a roadmap. And the new blood tests? Game-changers. I work in oncology and I’ve seen patients go from terminal to stable because they got screened early. If you’re over 50 and had sudden diabetes, or unexplained weight loss, or back pain that won’t quit - don’t wait. Push for an EUS. Ask for CA-19-9 + TIMP1 + LRG1 combo if your doc doesn’t know about it. Knowledge is power. And right now, that power is in your hands.
steve sunio
February 16, 2026 AT 18:57lol so you’re telling me i should get a $5000 scan because i lost 8 lbs and got tired? my grandma had that and lived to 92. you guys are so scared of cancer you think every sneeze is a tumor. also why do you say ‘early detection’ like its magic? it just means you get chemo 6 months earlier. same outcome. just more bills.
Neha Motiwala
February 18, 2026 AT 17:47I knew someone who died of this. She was 48. She went to the doctor 7 times. Said she had back pain. Said she was tired. Said she couldn’t eat. They gave her Zantac. Then she got jaundice. Then they found it. Stage IV. She cried every night. I cried every night. And now? Now I’m scared to eat. I don’t trust my body anymore. I don’t trust doctors. I don’t trust my own gut. If I lose a pound? I Google ‘pancreatic cancer symptoms’ at 3am. I don’t sleep. I don’t live. I just wait. For the next sign. The next whisper. The next death sentence.
Craig Staszak
February 19, 2026 AT 12:27I’ve been reading this whole thing and honestly I think the real issue isn’t the cancer - it’s that we’re too obsessed with early detection. What if we focused on making people feel better while they’re sick instead of panicking over a blood test? I’m not saying ignore symptoms. I’m saying maybe we’re overmedicalizing normal aging. My dad had weight loss and back pain at 67. He lived 10 more years. He didn’t need a scan. He needed a good meal and a nap.
alex clo
February 20, 2026 AT 01:24Thank you for compiling this with such precision. The data on neoadjuvant FOLFIRINOX and the emerging multi-marker panels like ESPAC are particularly compelling. As a medical professional, I can confirm that centers implementing these protocols have seen measurable improvements in resection rates and survival. The key is systematic screening for high-risk populations - not blanket testing. Genetic counseling should be integrated into primary care for those with family histories. This isn’t fearmongering - it’s evidence-based prevention.
Alyssa Williams
February 20, 2026 AT 08:41I’m a nurse and I’ve seen this too many times. A woman came in last month - 52, no family history, never smoked. Lost 12 lbs, new diabetes, always nauseous. Said her PCP told her it was ‘menopause.’ I pushed for an ultrasound. Tumor the size of a lemon. She’s in surgery next week. Don’t let anyone dismiss you. If you feel it in your bones - even if it’s just ‘off’ - keep asking. You are your best advocate. And if you’re scared? That’s okay. But don’t stay scared. Act.
Jack Havard
February 21, 2026 AT 20:20Why are we assuming the cancer is the enemy? What if it’s the body’s way of saying something’s wrong with the system? The pancreas doesn’t just ‘get cancer’ outta nowhere. It’s the toxins, the sugar, the stress, the lies we’re told about health. All these ‘breakthroughs’ are just band-aids. They’re selling tests and chemo and drugs. But no one talks about diet. No one talks about sleep. No one talks about the fact that people in rural India and Nigeria rarely get this cancer. Coincidence? I think not.