Every year, more than 1.5 million people in the U.S. are harmed by medications they took exactly as prescribed. That’s not a rare accident. It’s a system-wide problem - and most of it is preventable. If you or someone you love takes even one prescription, this isn’t just background noise. It’s your reality.
How Common Are Medication Errors?
One in every 20 patients worldwide suffers harm from a medication error. That means if you walk into a hospital, clinic, or even pick up a prescription at your local pharmacy, you have a 5% chance of being hurt by something meant to help you. In the U.S., that translates to over 1.3 million people injured each year. Some of these errors lead to hospital visits. Others lead to permanent damage. And about 7,000 people die in U.S. hospitals alone every year because of mistakes with drugs.
It’s not just hospitals. About 2% to 33% of patients make mistakes at home - taking the wrong dose, mixing pills they shouldn’t, skipping doses, or not realizing a new side effect is dangerous. A recent analysis of patient forums found that nearly 7 out of 10 people are confused about how to take their meds. That’s not their fault. It’s because instructions are unclear, labels are hard to read, or doctors don’t explain risks well enough.
Which Drugs Are Most Dangerous?
Not all medications carry the same risk. Some are far more likely to cause harm than others. Antibiotics top the list, responsible for about 20% of all medication-related injuries. Why? Because they’re overprescribed, misused, or given in the wrong dose. Antipsychotics come in second (19%), especially for older adults. These drugs are often used to calm dementia patients - even though guidelines say they shouldn’t be. Central nervous system drugs (16%) and heart medications (15%) are also high-risk.
But the scariest trend? Counterfeit drugs. In 2023, the DEA seized over 80 million fake pills - most of them laced with fentanyl. These aren’t street drugs. They’re sold online as oxycodone, Xanax, or Adderall. People think they’re buying real medicine. They’re not. In 2021, more than half of all overdose deaths from prescription painkillers involved fake pills. Fentanyl is now the leading cause of death for Americans between 18 and 45.
Who’s Most at Risk?
Older adults are the most vulnerable. They often take five, ten, or even more medications at once. Each new drug increases the chance of a bad interaction. In Australia, doctors cut the number of antipsychotics given to seniors by 11% in just five years - and saw fewer hospital stays as a result.
Children are also at risk. A parent might misread a dosage label. A nurse might accidentally give a child an adult dose. Even small mistakes can be deadly. And then there’s the rise in prescription stimulant misuse. Nearly 4 million Americans aged 12 and up reported using Adderall or Ritalin without a prescription in 2021 - mostly to stay awake or get high. That’s not just abuse. It’s a safety crisis.

Where Do Errors Happen?
Most errors happen at the point of care - when a drug is prescribed, dispensed, or given. But the biggest danger zone? Intravenous (IV) medications. In hospitals and nursing homes, nearly half of all medication errors involve IV drugs. One wrong decimal point - giving 10 milligrams instead of 1 - can kill someone.
Infusion pumps, the machines that deliver IV drugs, are another major problem. Between January 2023 and August 2024, over 200,000 pump-related events were reported to the FDA. That includes 204 deaths and nearly 2,000 injuries. These aren’t random glitches. They’re design flaws, poor training, or ignored alarms.
What Are Hospitals and Governments Doing?
Some places are making real progress. Australia launched 16 targeted actions to cut medication harm by half by 2025. So far, they’ve reduced opioid deaths by 37% using real-time prescription tracking. They’ve cut insulin-related emergencies by 10%. And they’ve stopped giving antipsychotics to seniors when they’re not needed.
In the U.S., Medicare is now tracking 16 safety measures for 2025 - from how well patients take their blood pressure meds to whether they’re getting unnecessary opioids. The FDA requires special safety plans for high-risk drugs. The EU now demands tamper-proof packaging on all prescription meds.
But here’s the hard truth: most of these efforts are still too slow. And they focus on systems, not patients. As Dr. Donald Berwick, a top patient safety expert, said: “Most errors aren’t because someone was careless. They’re because the system was broken.”
What You Can Do to Protect Yourself
You can’t fix the system alone. But you can protect yourself. Here’s how:
- Keep a live list of every medication you take. Include pills, vitamins, supplements, and creams. Update it every time your doctor changes something. Carry it with you - in your phone or wallet.
- Use one pharmacy for everything. Pharmacists can spot dangerous interactions between drugs. If you use multiple pharmacies, they can’t see the full picture.
- Ask the “Five Questions” every time you get a new prescription:
- What is this for?
- How and when do I take it?
- What side effects should I watch for?
- What happens if I miss a dose?
- Is there a cheaper or safer alternative?
- Check the pill before you leave the pharmacy. Does it look like the last one you got? If it’s a different color, shape, or size - ask why.
- Never take someone else’s meds - even if they have the same condition. Your body reacts differently. What’s safe for them could kill you.
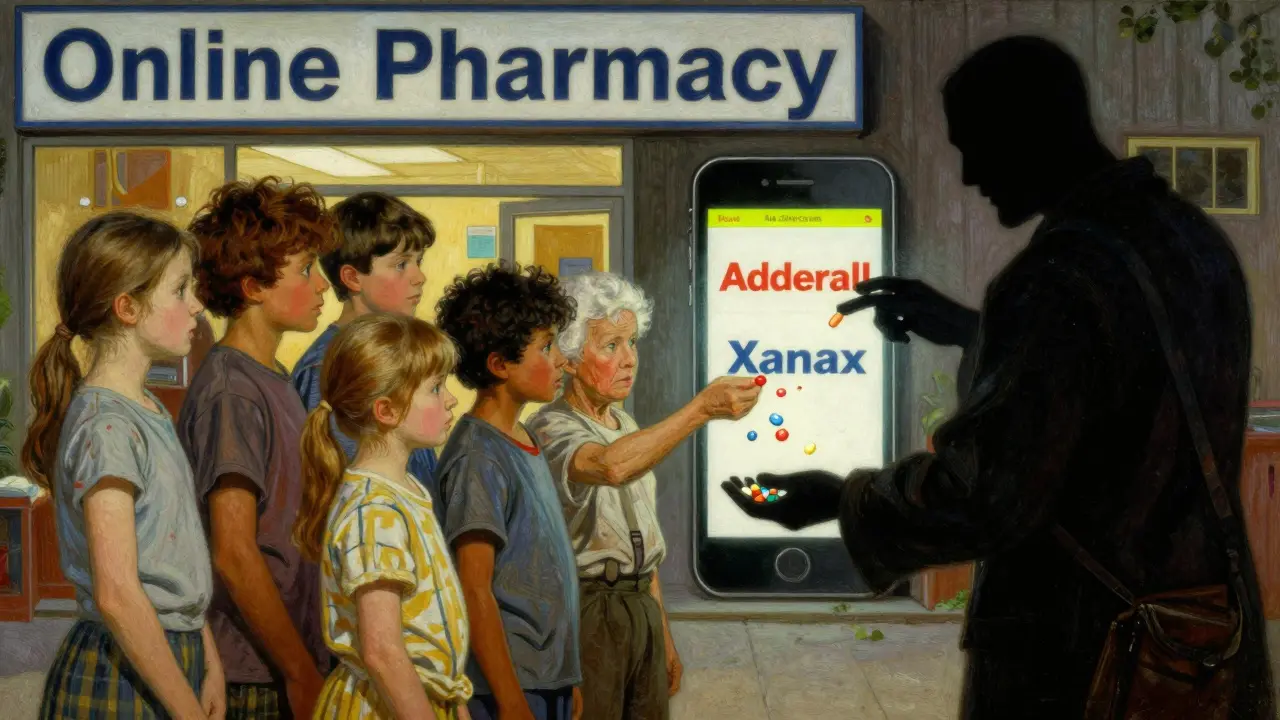
The Hidden Danger: Online Pharmacies
Buying pills online sounds easy. But 9 out of 10 websites selling prescription drugs are illegal. They don’t require prescriptions. They don’t check your health history. And they often sell fake, contaminated, or expired drugs.
Facebook, Instagram, and TikTok are now major markets for counterfeit pills. Ads promise “same-day delivery” for Xanax or Adderall. The pills look real. But they’re often packed with fentanyl - sometimes in doses strong enough to kill in seconds. The DEA says 1 in 5 counterfeit pills contains a lethal dose.
If you need a medication and can’t afford it, talk to your doctor. Ask about patient assistance programs. Use a licensed online pharmacy - one that requires a prescription and has a verified pharmacy seal. If it looks too good to be true, it is.
The Future of Medication Safety
Technology can help. AI tools are being tested to catch errors before they happen - like flagging a drug that shouldn’t be mixed with another, or spotting a dose that’s too high for an elderly patient. One study predicts these tools could reduce mistakes by 30% by 2027.
But tech alone won’t fix this. Patients need to be active partners. Doctors need time to explain. Pharmacies need better systems. Governments need to enforce rules - not just write them.
Right now, the odds are stacked against you. But you’re not powerless. The same system that harms you can be changed - if enough people speak up, ask questions, and demand better.
Medication safety isn’t just a hospital policy. It’s your right. And you’re the most important person in the chain that keeps you safe.
How many people are harmed by medications each year in the U.S.?
More than 1.5 million Americans are injured by medication errors every year, and about 7,000 die in hospitals alone. These numbers come from the World Health Organization and the Academy of Managed Care Pharmacy. Many more are harmed at home through mistakes in dosing, mixing drugs, or taking expired or fake pills.
What are the most dangerous medications?
Antibiotics cause the most harm overall, followed by antipsychotics, central nervous system drugs, and cardiovascular medications. But the deadliest trend is counterfeit pills - especially fake oxycodone laced with fentanyl. These are responsible for over half of all prescription overdose deaths in recent years. Even common drugs like insulin or blood thinners can be deadly if given in the wrong dose.
Why are older adults more at risk?
Older adults often take multiple medications - sometimes 10 or more - for chronic conditions. Each new drug increases the chance of a harmful interaction. They’re also more sensitive to side effects. Many are prescribed antipsychotics for dementia, even though guidelines warn against it. These drugs can cause falls, confusion, and even sudden death.
Can I trust online pharmacies?
Only if they’re verified. Over 90% of online pharmacies selling prescription drugs are illegal. They don’t require prescriptions, don’t check your health history, and often sell fake or contaminated pills. Look for the VIPPS seal (Verified Internet Pharmacy Practice Sites) or buy only from pharmacies linked to your doctor or insurance. If a website offers “no prescription needed” or “overnight delivery,” avoid it.
What should I do if I think I’ve been harmed by a medication?
Call your doctor or pharmacist immediately. Write down what you took, when, and what happened. Keep the pill bottle and any packaging. Report the incident to the FDA’s MedWatch program. You can file a report online or by phone. Don’t wait - even if you feel fine now. Some side effects show up days or weeks later.
How can I reduce my risk at home?
Use a pill organizer with labeled compartments. Set phone alarms for doses. Never skip doses just because you feel better. Ask your pharmacist to review all your meds once a year. Keep a written list of every drug you take - including vitamins and supplements - and bring it to every appointment. Don’t be afraid to ask: “Is this really necessary?”


Sarthak Jain
December 15, 2025 AT 22:28bro this is wild i had no idea 1 in 20 people get hosed by meds like it’s some kinda raffle. i take 5 pills a day and i just assume the doc knows what they’re doin. turns out maybe they’re just guessin with a clipboard. also why is my pharmacy always outta stock but the fentanyl laced xanax bots on ig never are? 🤔
Edward Stevens
December 17, 2025 AT 10:28Oh wow, another ‘you’re dumb for not reading the 12-page insert’ article. Let me guess - the solution is ‘just ask more questions’ like that’s gonna fix the fact that your doctor has 7 minutes to explain 8 new scripts while your insurance denies the good stuff. Classic. Meanwhile, the real villain is the $200 pill that costs $2 in India and the CEOs laughing all the way to the Caymans.
Rich Robertson
December 17, 2025 AT 19:13Just came back from visiting my grandma in Texas. She’s on 11 meds. Her pharmacy gave her a new bottle of metformin that looked nothing like the last one - no one asked why. She just took it. That’s not negligence, that’s a system designed to fail. We treat elderly patients like broken machines that need a new part every Tuesday. We need human-centered design, not just more stickers on bottles.
Rulich Pretorius
December 19, 2025 AT 17:02Medication safety isn’t about more warnings or fancy apps. It’s about power. The patient is the only one who lives with the consequences, yet the system treats them as an afterthought. Doctors prescribe, pharmacists dispense, insurers approve - but the person swallowing the pill? They’re just a data point. Real change starts when we give patients agency, not just pamphlets.
Sinéad Griffin
December 20, 2025 AT 06:21FAKE PILLS ON TIKTOK?? 😱 I saw a post yesterday saying ‘Adderall for focus’ with a girl doing a dance with a blue pill. That’s not a pill - that’s a death wish wrapped in glitter. And they’re selling it like it’s a TikTok trend?? 🇺🇸 WE NEED TO BAN THESE PLATFORMS FROM SELLING DRUGS. #MedicationSafety #FentanylIsMurder 💀
Dwayne hiers
December 20, 2025 AT 16:13IV errors are the silent killer in hospitals. The FDA’s 200k+ pump events? That’s just what got reported. Most are never logged. The real issue is lack of interoperability between EHRs and infusion systems. Without closed-loop verification - where the EHR auto-confirms dose, patient, and drug - you’re just gambling with a syringe. We have the tech. We just don’t fund it.
Natalie Koeber
December 20, 2025 AT 16:56They don’t want you to know this - but the whole system is rigged. Big Pharma owns the FDA, the doctors, even the pill colors. That’s why your blood pressure med looks different every month - it’s a different batch from a different shell company. And the ‘verified’ pharmacy seals? Fake. They’re printed by the same people who make the counterfeit pills. Wake up.
Wade Mercer
December 21, 2025 AT 12:44People need to stop being lazy. If you can’t read a label, don’t take the pill. If you don’t know what you’re taking, don’t take it. I’ve seen too many folks blame the system when they won’t even open the bottle to read the tiny print. It’s not a conspiracy - it’s personal responsibility. And if you’re too busy to care, don’t be surprised when you end up in the ER.
jeremy carroll
December 22, 2025 AT 14:50hey i just wanna say - this stuff is scary but you’re not alone. i used to take 3 meds for anxiety and never asked questions. then i started writing down every dose and asking my pharmacist ‘is this really needed?’ turns out one was just a placebo. i felt so dumb… but also so empowered. you got this. one pill at a time 💪
Jonny Moran
December 24, 2025 AT 01:09My cousin in rural Alabama got a new script for insulin. The label said ‘10 units’ - but the bottle said ‘10 mL’. She took it all. Ended up in the hospital. No one caught it. That’s not a mistake - that’s a design flaw. We need universal pictograms, voice-assisted labels, and pharmacy staff who actually talk to patients. Tech helps, but humanity matters more.
Tim Bartik
December 25, 2025 AT 06:35AMERICA IS THE BEST AT THIS SHIT. WE’VE GOT MORE DOCTORS, MORE PHARMACISTS, MORE TECHNOLOGY THAN ANY COUNTRY ON EARTH. IF YOU’RE GETTING HURT BY MEDS, IT’S BECAUSE YOU’RE TOO LAZY TO READ THE INSTRUCTIONS. STOP BLAMING THE SYSTEM - BLAME THE PEOPLE WHO DON’T CARE ENOUGH TO PAY ATTENTION. #AMERICA #MEDICATIONSAFETY #WAKEUP