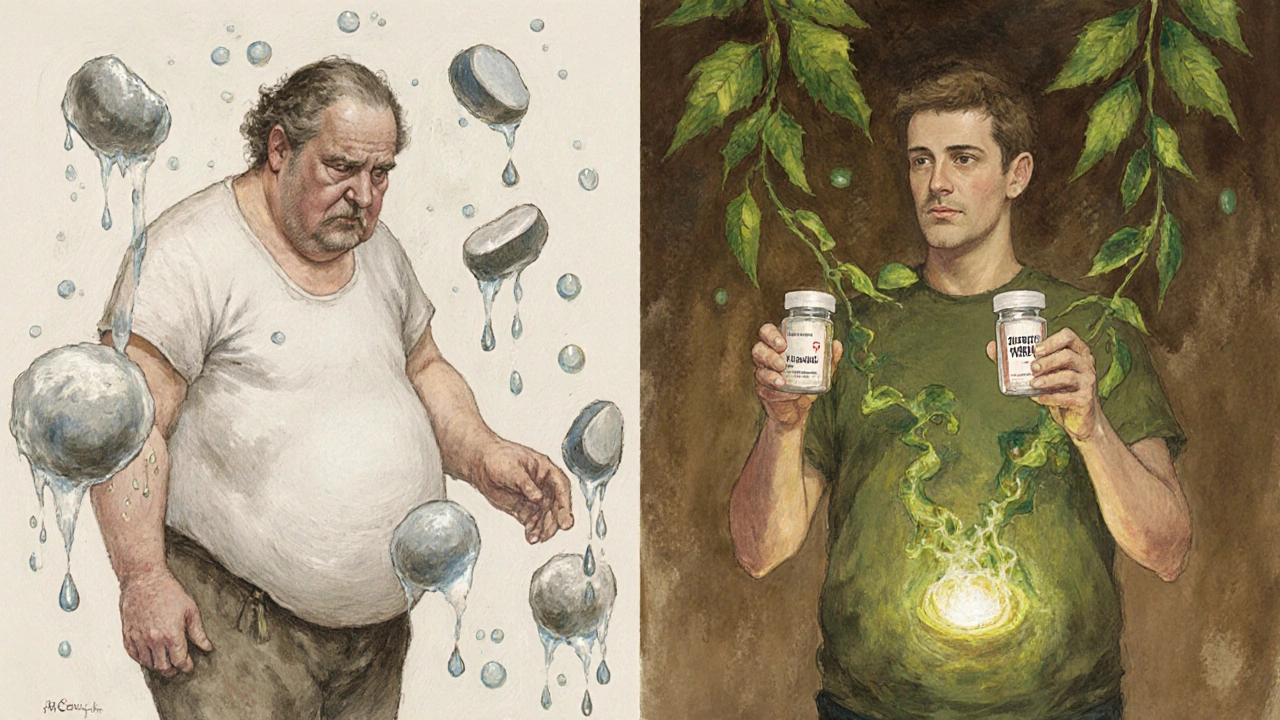
Many people start a new medication expecting to feel better - not to gain or lose pounds. But weight changes from drugs are more common than you think. In fact, about one in four prescription medications can shift your weight, sometimes without you realizing why. It’s not just about eating more or skipping the gym. It’s biology. Your body reacts to chemicals in pills in ways that alter appetite, metabolism, fluid balance, and even how much you move. And if no one warns you, you could gain 10, 15, even 20 pounds before you connect the dots.
Why Do Medications Change Your Weight?
It’s not magic. It’s science. Drugs interact with your brain, hormones, and fat cells in specific ways. There are five main reasons why a pill might make you heavier or lighter.
- Appetite boost: Some meds, especially certain antidepressants and antipsychotics, mess with serotonin receptors in your brain. This tricks you into feeling hungrier, even when you’re not. For example, mirtazapine increases cravings for carbs and snacks - studies show users gain 2-5 kg in just six months.
- Fat storage activation: Drugs like pioglitazone (used for type 2 diabetes) turn on PPAR-γ receptors, which tell your body to make more fat cells. In some cases, this increases fat storage by 40-60%.
- Slowed metabolism: Beta-blockers like propranolol, often prescribed for high blood pressure or anxiety, can drop your resting metabolic rate by 8-10%. That means you burn fewer calories just sitting still.
- Water retention: Steroids like prednisone cause your body to hold onto salt and water. It’s not fat - it’s fluid. But it can add 2-5 kg quickly, especially in the first month.
- Less movement: Antipsychotics and some sedatives make you tired. One Mayo Clinic study found patients on these drugs took 1,200 to 2,500 fewer steps a day. Less movement = fewer calories burned.
These effects aren’t random. They’re built into the drug’s design. A medication that calms your mood might also make you crave food. One that lowers blood sugar might also make you gain weight. That’s why choosing the right drug matters - not just for your condition, but for your body.
Which Medications Cause Weight Gain?
Not all drugs affect weight the same way. Some are notorious. Others barely touch it. Here’s what the data shows.
Antidepressants: SSRIs like paroxetine and sertraline often lead to 2.5-3.5 kg of weight gain over a year. Mirtazapine? Even worse - up to 5 kg in six months. But bupropion is different. It’s one of the few antidepressants that tends to cause weight loss, averaging 1.5-2.5 kg off over time.
Antipsychotics: Olanzapine is one of the worst offenders. In the CATIE trial, patients gained 4.5-6.0 kg in just 10 weeks. Quetiapine and clozapine follow closely. But aripiprazole? Almost weight-neutral - most people gain less than 1 kg. The difference? It doesn’t strongly block H1 and 5-HT2C receptors, which are linked to hunger signals.
Diabetes drugs: Insulin and sulfonylureas like glimepiride make you gain 2-4 kg in the first year. That’s because they push glucose into your cells - and excess glucose becomes fat. But GLP-1 receptor agonists like semaglutide and liraglutide do the opposite. In the STEP trials, people lost 5-15% of their body weight in under two years. That’s 6-10 kg for many.
Other culprits: Corticosteroids (prednisone), some epilepsy meds (valproate), and even certain birth control pills can cause water weight or fat gain. Beta-blockers like metoprolol and atenolol slow metabolism. And don’t forget antihistamines - they’re in many cold and allergy meds and can increase appetite.
Which Medications Help You Lose Weight?
It’s not all bad news. Some medications were designed to help you lose weight - or they just happen to.
GLP-1 receptor agonists are the biggest success story. Semaglutide (Wegovy, Ozempic), liraglutide (Saxenda), and tirzepatide (Zepbound) work by slowing stomach emptying, reducing hunger, and increasing fullness. In clinical trials, users lost 10-20% of their body weight. That’s not a fluke - it’s predictable.
Bupropion (Wellbutrin), used for depression and smoking cessation, also helps. It blocks dopamine and norepinephrine reuptake, which can suppress appetite. Studies show it leads to modest but consistent weight loss - especially when paired with lifestyle changes.
Even some diabetes meds like metformin can cause a small but meaningful weight loss of 2-4 kg over a year. It doesn’t burn fat directly, but it helps your body use insulin better - which reduces fat storage.
And here’s something new: combination drugs like Xultophy (insulin degludec + liraglutide) are being used to treat type 2 diabetes without the weight gain that usually comes with insulin. In the DUAL VIII trial, patients on this combo lost 4.2 kg more than those on insulin alone.
What Happens When You Take Multiple Weight-Gaining Drugs?
Most people don’t take just one medication. A 65-year-old with high blood pressure, diabetes, and depression might be on five or six pills. And if each one adds a little weight, the total adds up fast.
Dr. David Arterburn from Kaiser Permanente found that people on three or more weight-promoting drugs can gain 10-15 kg over five years. That’s not just inconvenient - it’s dangerous. Every extra 5 kg of weight gained increases heart disease risk by 12-18%, according to the Framingham Heart Study. For someone already overweight, this can push them into obesity.
It’s called the “polypharmacy weight trap.” And it’s often invisible until it’s too late. A patient might be doing great on their blood pressure meds, their antidepressant, and their diabetes drug - but slowly gaining weight with no one connecting the dots.
How to Manage Weight Changes from Medications
You don’t have to accept weight gain as part of treatment. There are smart ways to manage it.
- Start with a baseline: Before starting any new medication, get your weight and BMI recorded. This gives you a reference point. If you gain 2.5 kg or more in the first three months, it’s time to talk.
- Ask about alternatives: If you’re being prescribed a drug known for weight gain - like mirtazapine or olanzapine - ask: “Is there a similar option that doesn’t cause this side effect?” For depression, bupropion or sertraline might be better. For psychosis, aripiprazole is often a lighter choice.
- Track your weight monthly: Weigh yourself at the same time each week. Use a scale that measures body fat if possible. If you’re gaining more than 1 kg per month, it’s a red flag.
- Get nutritional support: A registered dietitian can help you adjust your diet without feeling deprived. Focus on protein, fiber, and whole foods. Avoid sugary drinks and processed snacks - they worsen the effect of appetite-stimulating drugs.
- Move more, even a little: If you’re tired from meds, start with 10-minute walks after meals. Gradually build to 30 minutes a day. Studies show even small increases in activity can offset metabolic slowdown.
- Consider weight-neutral options: For diabetes, GLP-1 drugs are now first-line for many patients - not just because they help with weight, but because they protect the heart. For high blood pressure, ACE inhibitors or ARBs are less likely to cause weight gain than beta-blockers.
And don’t wait until you’ve gained 10 kg. The Endocrine Society recommends intervention if you gain more than 2.5 kg in the first six months of treatment. Early action prevents long-term problems.
What Patients Are Saying
Real people are dealing with this every day.
On Reddit, one user wrote: “I gained 18 pounds on sertraline. I didn’t change my diet or exercise. I felt like I was losing control of my body. I switched to bupropion - and lost it all in four months.”
Another on HealthUnlocked said: “Switching from insulin to semaglutide didn’t just help my blood sugar - it helped me feel like myself again. I lost 22 pounds. My clothes fit. I slept better. I stopped dreading the scale.”
But not everyone feels heard. A 2024 survey found only 38% of patients were told about possible weight changes before their doctor prescribed the drug. That’s a gap. You have the right to know.
What’s Changing in 2025?
Things are getting better - slowly.
The FDA now requires drug makers to report exact weight changes in clinical trials, down to the gram per kilogram of body weight. That’s new. It means better data for doctors.
Genetic testing is starting to help too. Companies like Genomind offer panels that check your HTR2C gene variant - which predicts whether you’re likely to gain weight on antipsychotics. If you have the high-risk version, your doctor can choose a safer drug from the start.
And hospitals are waking up. By 2025, 87% of U.S. academic medical centers will require a metabolic risk assessment before prescribing psychiatric or diabetes drugs. That means weight won’t be an afterthought - it’ll be part of the decision.
The NIH just launched a $150 million initiative to develop 10 new weight-neutral medications by 2029. That’s a big step toward fixing the problem at the source.
Final Thoughts: You’re Not Alone, and It’s Not Your Fault
If you’ve gained weight on a medication, it’s not because you lack willpower. It’s because the drug changed your biology. And if you’ve lost weight on a drug, it’s not because you’re “better” - it’s because the chemistry worked differently.
The goal isn’t to stop taking your meds. It’s to take the right ones - and manage the side effects before they take over your life. Talk to your doctor. Ask questions. Bring your weight logs. Demand alternatives if you need them.
Medications are tools. They should help you live better - not make you feel trapped in your own body. You deserve to feel healthy in every way - mentally, physically, and emotionally.
Can antidepressants really cause weight gain?
Yes, many can. SSRIs like paroxetine and sertraline often lead to 2.5-3.5 kg of weight gain over a year. Mirtazapine is especially known for this - users may gain up to 5 kg in six months. But not all antidepressants do this. Bupropion tends to cause weight loss, and some people see no change at all. It depends on the drug and your body’s response.
Do diabetes medications cause weight gain?
Some do, some don’t. Insulin and sulfonylureas like glimepiride often cause 2-4 kg of weight gain in the first year because they push glucose into fat cells. But GLP-1 agonists like semaglutide and liraglutide cause weight loss - often 6-10 kg over a year. Metformin may lead to a small loss of 2-4 kg. The key is choosing the right drug for your body.
How do I know if my weight gain is from medication?
Track your weight before and after starting the drug. If you gain more than 1 kg per month without changing your diet or activity, it’s likely related. Check if the drug is known for weight gain - like antipsychotics, steroids, or certain antidepressants. Talk to your doctor. They can compare your medication profile with known side effects and suggest alternatives.
Can I switch medications if I’m gaining weight?
Yes - but don’t stop taking your meds on your own. Work with your doctor. For example, if you’re on olanzapine and gaining weight, switching to aripiprazole may help. If you’re on mirtazapine, bupropion might be a better option for depression. For diabetes, switching from insulin to a GLP-1 drug can reverse weight gain. The goal is to find a balance between effectiveness and side effects.
Is weight loss from drugs like Ozempic safe?
GLP-1 drugs like semaglutide (Ozempic, Wegovy) are FDA-approved for weight loss and diabetes. They’re safe for most people when used as directed. Side effects like nausea or diarrhea are common at first but usually fade. Long-term studies show they reduce heart attacks and strokes in high-risk patients. But they’re not for everyone - people with a history of thyroid cancer or pancreatitis should avoid them. Always use under medical supervision.
What should I ask my doctor before starting a new medication?
Ask: “What are the most common side effects, especially around weight?” “Is there a similar drug that doesn’t cause weight gain?” “Will this affect my appetite or metabolism?” “Can we check my weight before and after starting?” “Do you recommend a dietitian or fitness plan to help manage this?” If they brush you off, get a second opinion. Your weight matters.


Michael Petesch
November 19, 2025 AT 07:40The science here is solid, but what's missing is the systemic failure of prescribers to educate patients. This isn't just about biology-it's about a healthcare system that treats weight as a moral issue rather than a pharmacological one. Patients are left to guess why their clothes don't fit anymore, while doctors move on to the next chart. We need mandatory counseling on metabolic side effects, not just a footnote in a pamphlet.
Reema Al-Zaheri
November 19, 2025 AT 12:28It is essential to recognize that the pharmacological mechanisms described are not speculative-they are empirically validated through peer-reviewed clinical trials. The PPAR-γ receptor activation by pioglitazone, for instance, has been documented in at least seven randomized controlled studies since 2010. Similarly, the 5-HT2C antagonism linked to increased appetite is a well-established pathway in neuropharmacology. This is not anecdotal; it is evidence-based medicine.
Michael Salmon
November 19, 2025 AT 13:49Of course drugs cause weight gain. People don’t get fat because of biology-they get fat because they’re lazy. You think semaglutide makes you lose weight? No, it makes you stop eating like a pig. If you can’t control your appetite without a $1,000 monthly shot, maybe the problem isn’t the medication-it’s your discipline.
Christopher Robinson
November 20, 2025 AT 14:33Big thanks for this breakdown 🙏. I’ve been on metoprolol for 3 years and gained 15 lbs without changing a thing. No one ever told me it could do this. I’m going to ask my doc about ARBs next visit. Also-GLP-1s are game changers. My cousin lost 40 lbs on Ozempic and finally stopped hiding from family photos. It’s not magic. It’s science. And we need more of it.
James Ó Nuanáin
November 22, 2025 AT 12:08As a British physician with over two decades in clinical practice, I must emphasize that the American tendency to medicalize weight is both alarming and economically unsustainable. In the NHS, we do not prescribe weight-loss drugs as first-line therapy for depression. We prescribe therapy, lifestyle intervention, and, when necessary, bupropion-not Ozempic. This is not healthcare; it is pharmaceutical marketing masquerading as science.
Angela Gutschwager
November 22, 2025 AT 14:03I gained 20 lbs on sertraline. Switched to bupropion. Lost it all. No magic. Just chemistry. Stop blaming yourself.
Andy Feltus
November 23, 2025 AT 07:52Here’s the uncomfortable truth: We treat weight like a personal failure, but it’s often a pharmacological accident. We don’t scold someone for gaining weight from steroids after a transplant. We don’t tell a cancer patient to ‘just eat less’ when chemo makes them bloated. But if you’re on an antidepressant? Suddenly it’s your fault. That’s not medicine. That’s stigma dressed in white coats.
harenee hanapi
November 24, 2025 AT 08:32Oh my god, I knew it! I’ve been saying this for years! My psychiatrist prescribed me olanzapine and I gained 30 pounds in 4 months and no one listened! I cried in the grocery store because I couldn’t fit into my jeans and they just said ‘maybe try yoga’? Yoga?! I was on an antipsychotic! I had to change doctors and now I’m on aripiprazole and I’m finally breathing again. But why did it take me two years to find someone who believed me? Why is this so hard?
Timothy Reed
November 25, 2025 AT 23:05This is one of the clearest, most practical guides I’ve read on this topic. The six-step management plan is spot-on. I’ve seen too many patients fall into the polypharmacy weight trap-especially elderly folks on blood pressure meds, antidepressants, and diabetes drugs. The solution isn’t stopping meds-it’s smarter prescribing. Doctors need better tools, and patients need to be empowered to ask: ‘Is there a weight-neutral alternative?’ Simple. Effective. Long overdue.
Derron Vanderpoel
November 27, 2025 AT 06:35i just wanna say… i gained 18lbs on mirtazapine and i thought i was just lazy… but then i read this and i realized… it wasnt me… it was the pill… i switched to sertraline and i’ve lost 12lbs in 5 months… and i feel like me again… thank you for writing this… i’m not alone…
seamus moginie
November 28, 2025 AT 00:05It’s not about weight. It’s about autonomy. You’re told to take a pill to fix your brain, and suddenly your body betrays you. No warning. No consent. No choice. This isn’t treatment-it’s chemical coercion disguised as care. And the worst part? The system rewards doctors who prescribe the most profitable drugs, not the safest ones. You think this is about science? It’s about profit. And you’re the cash register.
Nick Lesieur
November 28, 2025 AT 06:07soooo… if i’m on 5 meds and gained 20 lbs… it’s not my fault? so i can just sit here eating cheetos and blame the pills? cool. so now i’m a victim AND a lazy sack? thanks for the guilt trip, doc.
Kara Binning
November 29, 2025 AT 03:35I’m so tired of people acting like weight gain from meds is some new revelation. My mother was on prednisone for lupus in the 80s and gained 50 pounds. They called it ‘moon face.’ No one ever said it was ‘unhealthy’-they just said ‘that’s what happens.’ Now? We’re treating it like a moral crisis. The hypocrisy is staggering. We’re obsessed with weight, but we don’t care about the people behind it.
Joe Durham
November 30, 2025 AT 16:17Thank you for writing this with so much humanity. I’ve been on insulin for 12 years and gained 30 pounds. I thought I was failing. I didn’t know GLP-1s could reverse it. I just started liraglutide last month. I’ve lost 8 pounds. I’m not ‘cured’-but I feel like I’m being treated as a whole person, not just a number on a scale. That matters more than you know.
Steve and Charlie Maidment
December 2, 2025 AT 01:40Okay, but let’s be real-most people who read this are going to immediately Google ‘Ozempic for weight loss’ and try to get it on the black market. We’ve turned medical treatments into status symbols. People are now bragging about their GLP-1 prescriptions like they’re designer handbags. And meanwhile, the people who need these drugs for diabetes are getting priced out. This isn’t progress. It’s commodification. And it’s going to get ugly fast.