Medication Psychosis Risk Checker
Check Your Medication Risk
This tool helps you identify if your medications may cause psychosis and shows what to watch for. Do not rely on this for medical advice - always consult your doctor.
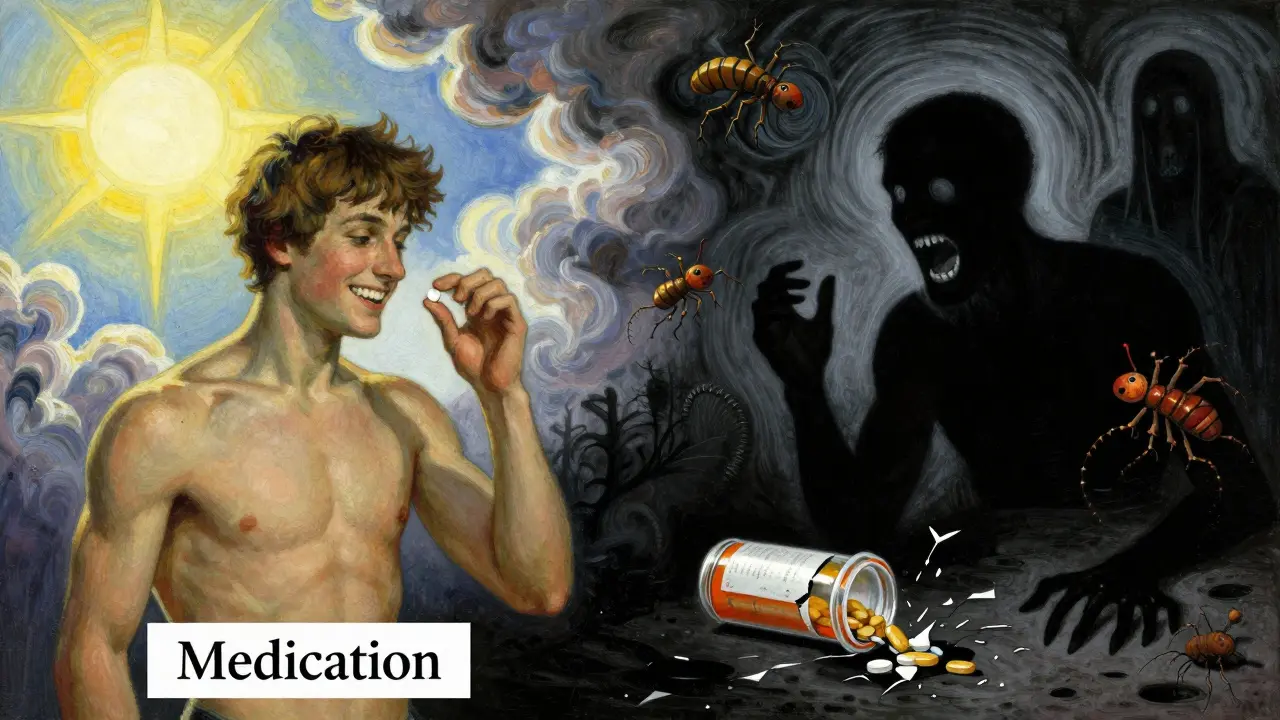
It’s not rare for someone to suddenly become paranoid, hear voices, or believe things that aren’t true-especially after starting a new medication. These aren’t just "bad side effects." They’re signs of medication-induced psychosis, a real and dangerous reaction that can happen with common drugs you might never suspect. Unlike schizophrenia or bipolar disorder, this isn’t a lifelong condition-it’s a medical emergency triggered by a drug, and it can flip a person’s reality in hours. The good news? If caught early, it usually goes away completely. The bad news? Many doctors miss it.
What Does Medication-Induced Psychosis Actually Look Like?
People experiencing this aren’t "going crazy." Their brain is reacting to a chemical change caused by a drug. The symptoms are unmistakable:
- Delusions-strong false beliefs, like thinking someone is spying on them or poisoning their food
- Hallucinations-seeing people who aren’t there, hearing voices whispering or yelling, feeling bugs crawling under the skin
- Disorganized speech-jumping between topics, saying things that don’t connect, using made-up words
- Severe confusion-forgetting where they are, not recognizing family members
- Extreme agitation or aggression-sudden outbursts, pacing, threatening behavior
- Mood swings-rapid shifts from panic to flat emotion
These aren’t vague feelings. They’re intense, persistent, and often terrifying-for the person experiencing them and everyone around them. Auditory hallucinations and paranoid delusions are the most common, especially with stimulants like cocaine or amphetamines. In fact, nearly 100% of heavy cocaine users who develop psychosis report hearing voices telling them they’re in danger.
Which Medications Can Cause This?
It’s not just illegal drugs. Many prescription and even over-the-counter medicines carry this risk. Here are the most common culprits:
- Corticosteroids (like prednisone)-used for asthma, arthritis, or autoimmune diseases. Up to 5.7% of people on high doses develop psychosis. Mood changes often come first-irritability, anxiety-before full hallucinations.
- Antimalarials (especially mefloquine)-used by travelers. The European Medicines Agency has logged over 1,200 psychosis cases since the 1980s. Nightmares and paranoia can start days after taking the first pill.
- Antiretrovirals (like efavirenz)-for HIV. About 2.3% of users report severe psychiatric side effects, including psychosis. The FDA requires warning labels.
- Antidepressants (SSRIs, SNRIs)-rare, but documented. Especially when starting or increasing the dose. Some people report sudden paranoia or delusions within days.
- Stimulants (methylphenidate, amphetamines)-used for ADHD. Psychosis occurs in over 11% of methamphetamine users and nearly 15% of amphetamine users.
- First-gen antihistamines (like diphenhydramine)-found in sleep aids and allergy pills. High doses can cause delirium and hallucinations, especially in older adults.
- Levodopa-for Parkinson’s. Can trigger hallucinations even at standard doses.
- Opioids and high-dose NSAIDs-less common, but possible, especially with long-term use or kidney problems.
And yes-even marijuana can do it. About 10% of regular cannabis users report psychotic symptoms, especially with high-THC strains. The key difference? If the hallucinations stop when the drug leaves the body, it’s likely medication-induced. If they stick around, it’s something else.
Who’s Most at Risk?
Not everyone who takes these drugs will develop psychosis. But certain people are far more vulnerable:
- People with a personal or family history of schizophrenia, bipolar disorder, or other psychotic illnesses
- Those with a history of substance use disorder-74% of first-time psychosis patients have had a past SUD
- Women-studies show higher rates of medication-induced psychosis in females, especially with steroids and antimalarials
- Older adults-slower metabolism means drugs stick around longer, increasing risk
- People with kidney or liver disease-can’t clear drugs properly
It’s also more likely if someone is taking multiple drugs at once. A person on prednisone for arthritis who also takes diphenhydramine for sleep? That combo can push someone over the edge.

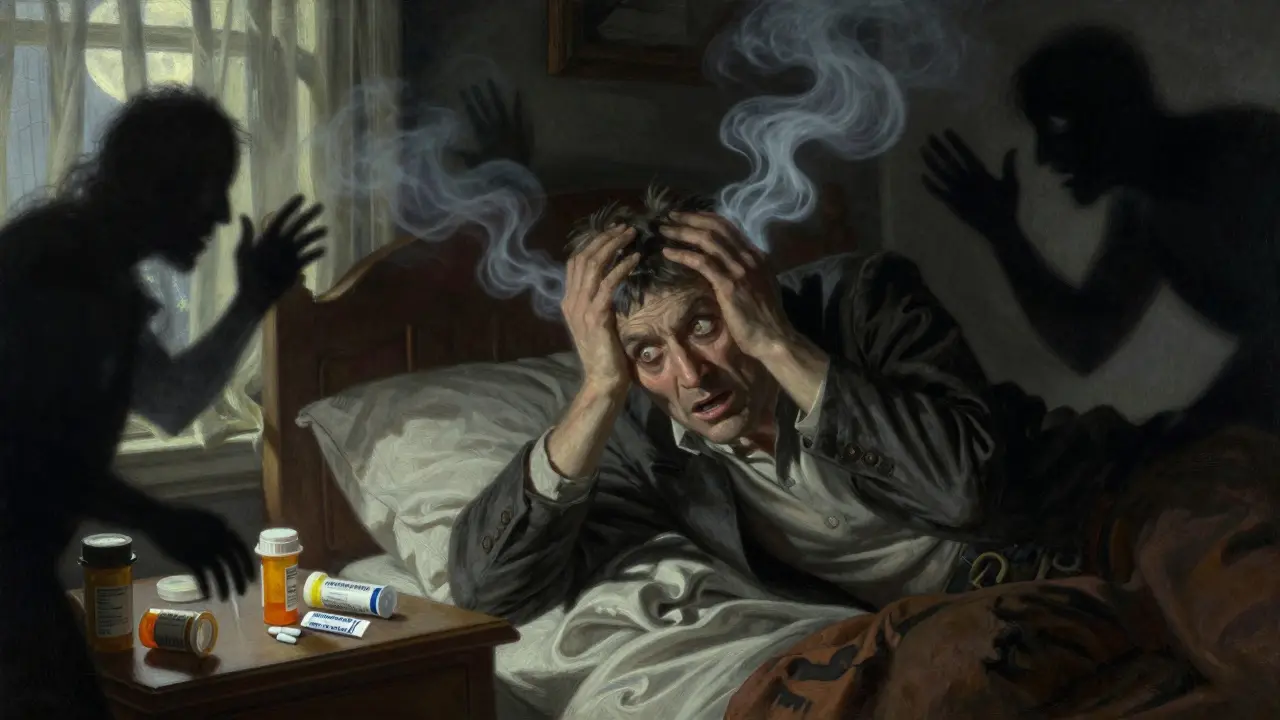
Emergency Management: What to Do Right Now
If someone suddenly becomes psychotic after starting a new medication, don’t wait. Don’t assume it’s "just stress." Call emergency services or go to the nearest ER immediately.
Here’s what happens in the emergency room:
- Stop the drug-The first and most important step. If it’s a prescription, the doctor will discontinue it. If it’s an OTC pill, they’ll confirm what was taken and how much.
- Stabilize the patient-If they’re agitated or violent, they may be given a short-acting antipsychotic like olanzapine or quetiapine. Benzodiazepines (like lorazepam) are also used to calm extreme anxiety or seizures.
- Rule out other causes-Doctors will check for infections, low blood sugar, electrolyte imbalances, or alcohol withdrawal-all can mimic psychosis.
- Monitor closely-They’ll watch for heart issues, high body temperature (especially with stimulants), or muscle breakdown (rhabdomyolysis).
For alcohol or benzo withdrawal psychosis, treatment is different. They’ll give a controlled taper of benzodiazepines to prevent delirium tremens-a life-threatening condition.
And yes-sometimes hospitalization is necessary. If someone is a danger to themselves or others, involuntary holds under mental health laws are legal and often lifesaving.
How Long Does It Last?
Recovery time depends on the drug:
- Cocaine or amphetamines-Symptoms often clear in 24 to 72 hours after last use
- Steroids-Take 4 to 6 weeks to fully resolve after stopping
- Antimalarials like mefloquine-Can take weeks, sometimes months, for brain chemistry to reset
- Antidepressants-Usually improve within 1 to 2 weeks of discontinuation
Most people recover fully. But here’s the catch: up to 10% of first-episode psychosis cases in ERs are medication-induced. That means nearly 1 in 10 people admitted for "new psychosis" actually had a drug trigger. If symptoms linger beyond a month after stopping the drug, doctors must consider an underlying psychotic disorder like schizophrenia.
Why This Gets Missed So Often
Primary care doctors miss it all the time. A 2019 study found only 38% felt confident diagnosing it. Why?
- They assume psychosis = schizophrenia
- They don’t ask about recent medication changes
- Patients don’t volunteer that they took an OTC sleep aid or started a new steroid
- Doctors don’t know which drugs carry this risk
It’s not their fault. The information isn’t always clear in drug labels. But it’s critical to ask: "When did this start? What new meds or supplements did you begin taking?"
How to Prevent It
Prevention is simple, but often ignored:
- Always tell your doctor about all medications, including OTC pills, supplements, and herbal products
- If you’re prescribed a drug known to cause psychosis (like steroids or mefloquine), ask: "What mental side effects should I watch for?"
- Don’t start new drugs without knowing the risks-read the FDA patient guide if one exists
- Monitor for early warning signs: anxiety, sleeplessness, irritability, racing thoughts-these often come before full psychosis
- If you have a psychiatric history, tell your doctor before starting any new medication
And if you’re caring for someone on high-risk meds-keep a close eye. A sudden change in behavior isn’t "just them." It could be the drug.
What Happens After the Emergency?
Once the acute phase passes, follow-up is non-negotiable. You need psychiatric care for at least 3 months. Why?
- To confirm the psychosis was truly drug-induced
- To watch for delayed onset of schizophrenia or bipolar disorder
- To address any substance use issues that may have contributed
- To help the person rebuild trust in their own mind
Some people need therapy to process the trauma of experiencing psychosis. Others need help quitting drugs or adjusting to life after stopping a medication they thought was helping them.
The bottom line: medication-induced psychosis is treatable, reversible, and often preventable. But it demands urgency. Ignoring it can lead to hospitalization, lost jobs, broken relationships, or worse. If you or someone you know starts acting strangely after a new drug-act fast. It’s not paranoia. It’s a medical alert.
Can over-the-counter meds cause psychosis?
Yes. First-generation antihistamines like diphenhydramine (found in Benadryl, sleep aids, and cold medicines) can cause hallucinations and delirium, especially at high doses or in older adults. Even large amounts of pseudoephedrine (in decongestants) have triggered psychosis in rare cases.
How is medication-induced psychosis different from schizophrenia?
The key difference is timing and duration. Medication-induced psychosis starts within a month of taking or stopping a drug and usually resolves within weeks after stopping it. Schizophrenia lasts longer than six months, often for life, and doesn’t go away just because you quit a medication. If symptoms persist after the drug is out of your system, it’s likely a primary disorder.
Is medication-induced psychosis permanent?
In most cases, no. When the drug is stopped and managed properly, symptoms fade. But with long-term, high-dose exposure-especially to stimulants or alcohol-some people develop lasting brain changes. In rare cases, the episode may trigger an underlying condition like schizophrenia, making it seem permanent when it’s actually a new diagnosis.
Can you get psychosis from stopping a medication?
Yes. Withdrawal from alcohol, benzodiazepines, and even some antidepressants can trigger psychosis. This is especially dangerous with alcohol or benzo withdrawal, which can escalate into delirium tremens-a medical emergency. Never stop these drugs cold turkey without medical supervision.
What should I do if I think my loved one is having medication-induced psychosis?
Stay calm, keep them safe, and call emergency services. Don’t argue with their delusions. Don’t try to reason with them. Gather a list of all medications they’ve taken in the past 30 days-including vitamins and supplements-and take it with you to the ER. Early action saves lives.

Janette Martens
December 29, 2025 AT 02:44stupid meds.
Marie-Pierre Gonzalez
December 29, 2025 AT 12:05It is imperative that all prescribers conduct thorough medication reconciliation - including OTCs and supplements - and educate patients on potential neuropsychiatric side effects prior to initiation. Early intervention saves lives, relationships, and careers.
With deepest respect for those affected and their families.
Louis Paré
December 30, 2025 AT 08:56Wow. What a shock. Next you’ll tell me water can drown people.
Every single one of these drugs has a warning label. If you don’t read the tiny print, you’re not a victim - you’re just lazy. And now we’re supposed to panic every time someone takes Benadryl?
People need to stop outsourcing responsibility for their own choices to Big Pharma.
Also, the fact that you included marijuana as a culprit but didn’t mention that 90% of users never have psychosis suggests you’re cherry-picking data to scare people.
Psychosis isn’t a bug - it’s a feature of weak minds.
James Hilton
December 31, 2025 AT 03:56she was fine 2 weeks after quitting.
why is this even a news story?
Mimi Bos
January 1, 2026 AT 16:04Payton Daily
January 1, 2026 AT 22:18are we just meat puppets controlled by chemistry?
if a drug can make you believe your neighbor is a robot spy, then isn’t every belief we have just a chemical accident?
if your thoughts can be hijacked by a prescription, then what’s real?
we’re all one pill away from madness.
and the system knows it.
they’re drugging us to keep us docile.
you think prednisone causes psychosis?
what about the 500 other chemicals in your food, water, air?
they’re all testing us.
and the ones who break?
they call it psychosis.
the rest of us?
we call it normal.
Kelsey Youmans
January 3, 2026 AT 19:56It is critical that primary care providers maintain a high index of suspicion, particularly in vulnerable populations such as the elderly and those with polypharmacy.
Documentation of medication timelines and patient education must be prioritized.
Thank you for highlighting this underrecognized public health issue with such clarity and precision.
Sydney Lee
January 5, 2026 AT 00:22Every single one of these drugs is aggressively marketed while their psychiatric risks are buried in the appendix of a 47-page FDA document.
Big Pharma doesn’t want you to know that your antidepressant might turn you into a paranoid shell.
They want you to take it for life.
And doctors? They’re complicit. They’re too busy checking boxes to ask, "When did this start?"
It’s not negligence - it’s profit-driven silence.
And now we’re left with families shattered, careers destroyed, and people branded as "crazy" when all they needed was to stop a pill.
What’s more dangerous? The drug - or the system that lets this happen over and over?
Julius Hader
January 5, 2026 AT 18:37they told me it was "stress".
nah.
they're covering it up.
Vu L
January 6, 2026 AT 22:05oluwarotimi w alaka
January 7, 2026 AT 08:44my cousin took malaria pills and started talking to the moon. now he's in a psych ward. coincidence?
i think not.
they're testing it on us.
and you're all just sitting here like sheep.