When you think of a generic drug, you picture a small pill that looks different but works the same as the brand-name version. That’s straightforward. But biosimilars? They’re not that simple. These aren’t just copies of a chemical formula-they’re living, breathing molecules made inside cells, shaped by temperature, pH, nutrients, and timing. Even a tiny shift in any of those factors can change how the drug behaves in your body. And that’s why manufacturing biosimilars is one of the most complex tasks in modern medicine.
The Core Problem: You Can’t Just Copy the Formula
Generics are made by mixing chemicals in a lab. If you know the recipe, you can make the exact same molecule every time. Biosimilars? They’re proteins-sometimes thousands of times bigger than a generic drug molecule-grown inside living cells like Chinese hamster ovary (CHO) cells. The cells don’t follow a recipe. They respond to their environment. Change the sugar in their food, the oxygen level in the tank, or the temperature by just one degree, and the final product changes. That’s why experts say: the process defines the product.You’re not just making a drug. You’re trying to recreate a biological fingerprint. And you don’t have the original recipe. The originator company keeps its exact process secret. So biosimilar makers have to reverse-engineer it. Think of it like trying to copy a Michelin-star dish without knowing the ingredients, the cook’s technique, or even what pan they used. You taste it, study it, test it, and then spend years tweaking your own kitchen until it’s close enough.
Glycosylation: The Silent Game-Changer
One of the biggest hurdles? Glycosylation. That’s when sugar molecules attach to the protein backbone of the biologic. It sounds technical, but it matters. These sugar chains affect how long the drug lasts in your bloodstream, how well it binds to its target, and whether your immune system reacts to it. A slight change in glycosylation can turn a safe, effective drug into one that’s cleared too fast-or worse, triggers an immune response.These sugars aren’t added by hand. They’re added by the cell’s own machinery. And that machinery is finicky. A change in the culture medium, a drop in dissolved oxygen, or even how fast the bioreactor spins can alter the glycan profile. Biosimilar manufacturers must match the reference product’s glycosylation pattern within strict limits-often less than 5% variation. That’s not easy. It requires hundreds of tests, advanced mass spectrometry, and years of process optimization.
Scaling Up: Bigger Tanks Don’t Mean Better Results
Getting a biosimilar to work in a 5-liter lab bioreactor is one thing. Scaling it to 10,000 liters for commercial use? That’s another world. In small tanks, mixing is even. Oxygen flows smoothly. Temperature stays steady. In big tanks? It’s messy. Some parts get more oxygen than others. Some cells get more nutrients. The result? Cells in different zones grow differently. The protein they produce isn’t uniform.Manufacturers have to re-engineer everything: how they stir the tank, how they pump in nutrients, how they control heat. It’s like trying to bake the same cake in a home oven and a commercial bakery oven-same recipe, different results. And there’s no shortcut. Each scale-up step requires new validation, new testing, and new regulatory approval. Many smaller companies can’t afford the capital to build or rent these massive facilities. That’s why only a handful of firms dominate the biosimilar market.
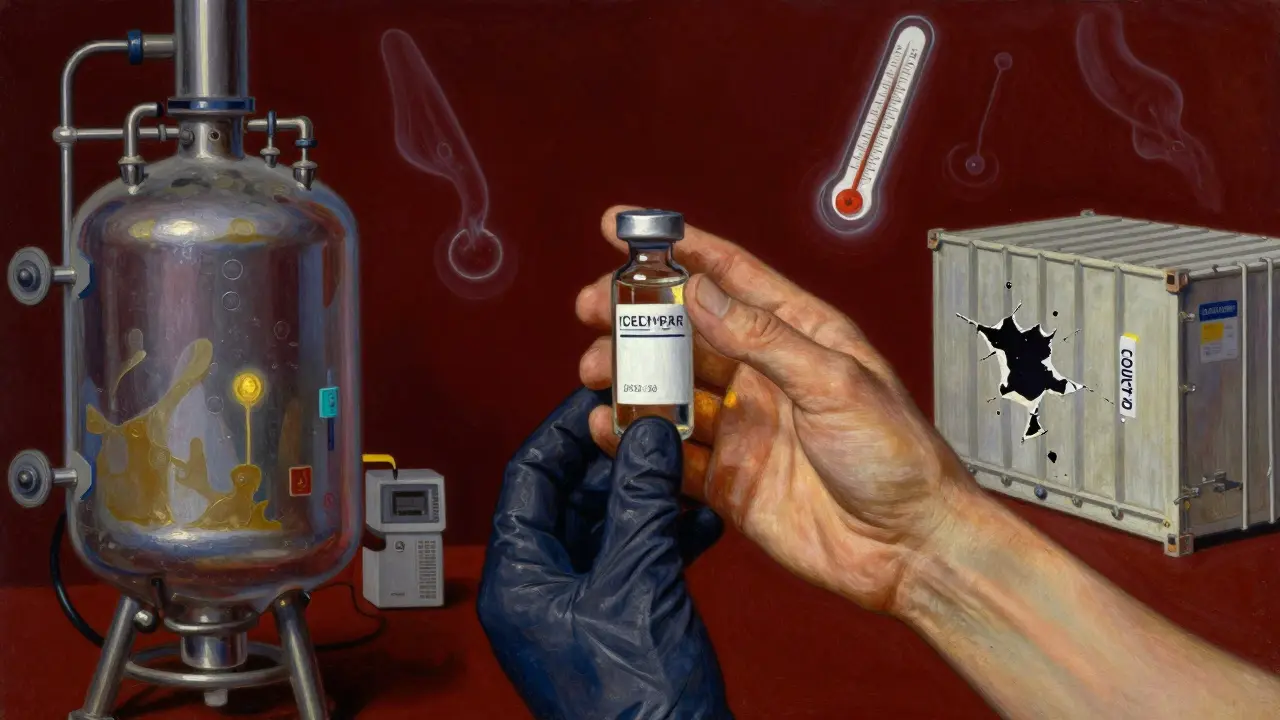
Cold Chain and Handling: One Mistake, Millions Lost
Biosimilars don’t just need careful production-they need careful handling. Most are stored and shipped frozen or refrigerated. If a shipping container’s temperature rises for even a few hours, the protein can unfold, clump, or degrade. That’s not just a quality issue-it’s a safety risk. A single damaged batch can cost millions. And because biosimilars are made in small batches compared to generics, there’s little room for error.Filling the final vials or syringes is another high-risk step. The liquid must be sterile, free of particles, and perfectly mixed. Any contamination or air bubble can ruin the batch. That’s why many manufacturers are switching to closed, automated systems. Robots handle the filling, reducing human error and contamination risk. But these systems are expensive. Smaller companies often can’t afford them.
Regulatory Maze: More Than Just a Paper Trail
Getting a biosimilar approved isn’t like submitting a generic drug application. You don’t just prove bioequivalence. You prove similarity across dozens of dimensions: structure, purity, stability, function, and even how it behaves in the body. Regulatory agencies like the FDA and EMA demand stacks of data-from atomic-level protein analysis to clinical trials comparing immune responses.And it’s not the same everywhere. The EU has been approving biosimilars for over 15 years. The U.S. is catching up. Other countries have their own rules. One batch might pass in Germany but get rejected in Brazil because of a different acceptance threshold for a specific impurity. Manufacturers need global regulatory expertise, not just lab skills. They need teams that know how to write dossiers, interpret guidelines, and respond to agency questions-all while keeping production running.

Technology Is Helping, But It’s Not a Magic Fix
There’s good news: new tools are making biosimilar manufacturing more manageable. Single-use bioreactors-disposable plastic tanks-are replacing stainless steel ones. They cut cleaning time, reduce cross-contamination, and let companies switch between products faster. Process Analytical Technology (PAT) lets manufacturers monitor critical parameters in real time. If the pH drifts, the system adjusts automatically. Artificial intelligence is being used to predict when a batch might fail before it happens.But these aren’t cheap. A single-use bioreactor system can cost over $2 million. PAT systems require specialized software and trained staff. AI models need years of data to train. So while these tools are game-changers, they’re still out of reach for many startups. The result? The market is consolidating. Big players with deep pockets are buying up smaller firms. The barrier to entry is getting higher, not lower.
The Future: More Complexity, More Pressure
The next wave of biosimilars won’t be simple monoclonal antibodies. They’ll be bispecific antibodies, antibody-drug conjugates, fusion proteins-molecules that are even more complex. These require extra steps: chemical conjugation, refolding, purification of multiple components. Each step adds risk. Each step needs validation. Each step increases cost.At the same time, pressure is rising to lower prices. Insurers and governments want biosimilars to cut costs. But if the manufacturing process is too expensive, the savings vanish. Companies are caught in a tight spot: make it cheaper, and risk quality. Make it perfect, and it’s too expensive to compete.
The answer isn’t just better tech. It’s better integration. Better data sharing between R&D and production. Better collaboration with regulators. Better training for operators. And above all, a deep understanding that biosimilars aren’t generics with a fancy name. They’re a different kind of medicine-built by living cells, shaped by invisible forces, and held together by precision, patience, and billions of dollars in investment.
Why This Matters for Patients
You might wonder: why should I care how hard it is to make these drugs? Because if the manufacturing fails, the supply fails. If a batch is rejected, there’s no backup. If a company can’t afford the equipment, it won’t make the drug at all. That means fewer options. Higher prices. Longer waits. And for patients who rely on biologics for conditions like rheumatoid arthritis, cancer, or Crohn’s disease, delays can be dangerous.Biosimilars were supposed to make life-saving treatments more affordable. But if the manufacturing hurdles are too high, they’ll stay out of reach for most of the world. The real challenge isn’t just science. It’s making sure that science reaches the people who need it.
Are biosimilars the same as generics?
No. Generics are chemically identical copies of small-molecule drugs. Biosimilars are highly similar-but not identical-to large, complex biologic drugs made from living cells. Because biologics are made by cells, not chemical reactions, even tiny differences in manufacturing can change how they work. That’s why biosimilars require far more testing than generics.
Why is glycosylation such a big deal in biosimilars?
Glycosylation refers to the sugar chains attached to protein-based biologics. These sugars affect how long the drug stays in your body, how well it binds to its target, and whether your immune system reacts to it. Even small changes in glycosylation can reduce effectiveness or cause side effects. Since these sugars are added by living cells-not chemists-controlling them is extremely difficult and requires precise, consistent manufacturing conditions.
Can biosimilars be made cheaper than the original biologics?
Yes, but not always. Biosimilars cost less to develop than new biologics, but manufacturing them is still extremely expensive-often hundreds of millions of dollars. The cost comes from complex processes, strict quality controls, and specialized equipment. While they’re typically 15-35% cheaper than the originator drug, they’re not as cheap as generics. Savings depend on scale, technology, and regulatory efficiency.
What’s the biggest barrier for new companies entering the biosimilars market?
The biggest barrier is capital. Building a biosimilar manufacturing facility requires massive investment in bioreactors, purification systems, analytical labs, and automation. Regulatory expertise and compliance costs are also high. Most new entrants lack the resources to meet global standards. As a result, the market is dominated by a few large biotech firms with decades of experience.
How do regulators ensure biosimilars are safe?
Regulators like the FDA and EMA require extensive testing: analytical studies to compare molecular structure, non-clinical studies to assess toxicity, and clinical trials to confirm safety and efficacy. They look at over 20 critical quality attributes, including purity, stability, and biological activity. Only after proving similarity across all these areas is a biosimilar approved. It’s a far more rigorous process than for generics.
Will biosimilars ever be as simple to make as generics?
Not likely. The complexity comes from the biology itself. As long as biosimilars are made using living cells, there will be inherent variability. Advances in AI, automation, and continuous manufacturing may reduce costs and improve consistency, but they won’t eliminate the need for deep biological understanding and tight process control. Biosimilars will always be more complex than generics.


Rachel Wermager
January 8, 2026 AT 07:07The glycosylation heterogeneity in biosimilars is the single most underappreciated bottleneck in biopharma. When you're dealing with N-glycan profiles that vary by sialylation, fucosylation, and galactosylation patterns, you're not just optimizing a process-you're dancing with stochastic biological noise. The FDA’s acceptance criteria for glycan similarity (≤5% deviation) is statistically rigorous but practically impossible to maintain at scale without real-time PAT systems and machine learning-driven process control. Most startups don’t even have the mass spec infrastructure to characterize this, let alone replicate it.
Tom Swinton
January 9, 2026 AT 22:18I just want to say-this is one of the most important things we’re not talking about enough. People think ‘generic’ means ‘cheap and easy,’ but biosimilars? They’re like trying to clone a symphony orchestra using only a recording and a bunch of mismatched instruments. Every single variable-from the pH of the nutrient broth to the humidity in the cleanroom-matters. And when a batch fails after 45 days of growth? That’s not just money lost. That’s a patient who might not get their next dose on time. I’ve seen families cry because a biosimilar was delayed. This isn’t just science-it’s humanity, wrapped in bioreactors and sterile filters.
Leonard Shit
January 10, 2026 AT 04:56so like… biosimilars are basically the biological version of trying to recreate your ex’s cooking after they ghosted you? you know the taste, you’ve seen the ingredients… but no matter how hard you try, it’s never quite the same? and then you spend $200M trying to make it work? yeah. i get it. 🤷♂️
Katelyn Slack
January 10, 2026 AT 10:27I’ve worked in pharma QA for 12 years and this post nailed it. The cold chain part? That’s the silent killer. One temperature excursion during shipping and the whole lot’s trash. No warning. No second chances. Just a $3M loss and a hospital waiting on a life-saving drug.
Melanie Clark
January 12, 2026 AT 09:32Big Pharma doesn’t want biosimilars to succeed because they’re scared of losing their monopoly. The ‘complexity’ is manufactured. The real reason they’re expensive is because the FDA lets them hide behind ‘proprietary processes’-but we all know it’s just a cover for price gouging. The same companies that made billions off Humira are now lobbying to block cheaper versions. It’s not science-it’s greed. And they’re using ‘glycosylation’ as a smokescreen.
Harshit Kansal
January 13, 2026 AT 06:50bro this is wild. in india we have a lot of generic makers but biosimilars? super hard. one company tried making a trastuzumab biosimilar and the glycosylation was off by 8%. they lost 10 crores. now they’re doing chai instead. 😅
Brian Anaz
January 13, 2026 AT 20:44USA makes the best drugs. Other countries can’t even handle the science. Why are we letting cheap foreign labs try to copy our biologics? They don’t even have clean rooms that meet our standards. This isn’t innovation-it’s outsourcing failure. We should ban imports until they prove they can do it right. America First in biotech.
Venkataramanan Viswanathan
January 14, 2026 AT 13:01In India, we have over 20 biosimilar manufacturers, but only 3 can consistently meet EMA standards. The gap isn’t in talent-it’s in infrastructure. We have brilliant scientists, but without access to single-use bioreactors or AI-driven PAT systems, we’re stuck playing catch-up with billion-dollar budgets. The world needs to invest in global equity, not just profit margins.
Vinayak Naik
January 15, 2026 AT 23:04yo the glycosylation thing is wild. it’s like the protein’s got a secret tattoo made of sugar that only the original company knows how to ink. you can try to trace it under a microscope but half the time you’re just guessing. and when the cells get stressed? they start adding extra sugar like it’s a party. chaos.
Kiran Plaha
January 17, 2026 AT 18:39So if biosimilars are so hard to make, why do we even bother? Isn’t it easier to just let the original companies keep pricing high?