Missing a dose of your medication happens to almost everyone at some point. Maybe you overslept. Maybe you were in a rush. Or maybe you just forgot because you’re juggling too many pills. The panic that follows is real: should I take two now to make up for it? The answer is almost always no-and here’s why.
Why Doubling Up Is Dangerous
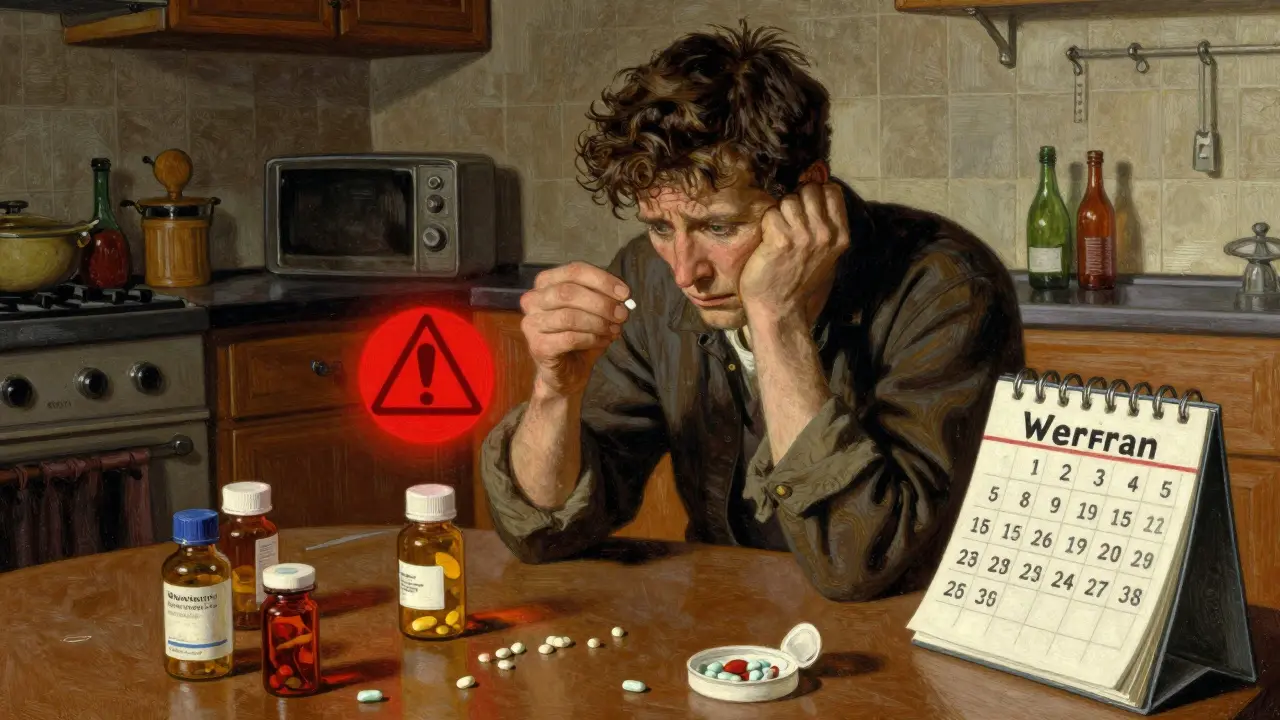
Taking two doses at once might seem like a quick fix, but it can be dangerous-or even life-threatening. Medications are designed to stay in your system at a steady level. When you double up, you spike that level suddenly. For some drugs, even a small overdose can cause serious harm. Take warfarin, for example. It’s a blood thinner used to prevent clots. Its therapeutic window is extremely narrow: too little, and you risk a stroke; too much, and you could bleed internally. A 2022 study in JAMA Internal Medicine found that 68.4% of patients who doubled their warfarin dose ended up with INR levels above 5.0-far beyond the safe range. That’s a direct path to emergency hospitalization. The same goes for digoxin (used for heart rhythm), antiepileptics like phenytoin, and even methotrexate (used for autoimmune conditions and cancer). These drugs have what’s called a narrow therapeutic index. That means the difference between a helpful dose and a toxic one is tiny. Doubling up isn’t just risky-it’s reckless.It’s Not One-Size-Fits-All
There’s no universal rule for every medication. What you do after missing a dose depends on the drug’s half-life, how often you take it, and its risk category. The National Patient Safety Agency (NPSA) classifies medications into three groups:- Red risk: High danger if missed or doubled. Includes anticoagulants, antiepileptics, insulin, and immunosuppressants.
- Amber risk: Moderate risk. Think blood pressure meds, some antidepressants.
- Green risk: Low risk. Most statins, some vitamins, and mild pain relievers.
Once-Daily Medications
If you take a pill once a day and realize you missed it:- If it’s still the same day, take it as soon as you remember.
- If it’s the next day, skip the missed dose. Don’t take two.
Twice-Daily Medications
For meds taken twice a day-say, 8 a.m. and 8 p.m.-you have a bit more flexibility.- If you miss the 8 a.m. dose and remember before 2 p.m., take it.
- If it’s after 2 p.m., skip it. Wait until your next dose at 8 p.m.

Special Cases: Birth Control and GLP-1 Drugs
Some medications need special handling. Oral contraceptives: If you miss an active pill by less than 12 hours, take it as soon as you remember. If it’s been more than 12 hours, take it when you remember-but use backup contraception (like condoms) for the next 7 days. The Australian Prescriber confirms this is the safest approach to maintain contraceptive effectiveness. GLP-1s like semaglutide or tirzepatide: These weight-loss and diabetes drugs are injected once a week. If you miss your dose, you can take it up to 4 days late. But if you miss two doses in a row (14 days without the drug), don’t just jump back in. Talk to your doctor. Clinical trial data shows 23.7% of patients experience nausea or vomiting when restarting after a long gap.What About Antibiotics?
This is one of the few exceptions. For some antibiotics like amoxicillin, taking a double dose if you miss one can be safe and even recommended-because you need high enough levels to kill bacteria. But this applies to less than 3% of all prescriptions. Never assume your antibiotic is one of them. Always check the leaflet or call your pharmacist.Why So Much Confusion?
You’re not alone if you’re unsure. A 2021 review found that 25% of high-risk medications had no missed-dose instructions in their official patient leaflets. Even worse, 41.7% of leaflets gave conflicting or unclear advice. One patient on Trustpilot shared: “I was told three different things about my blood pressure meds by three different pharmacies.” That’s not rare. Pharmacists are human. They’re busy. And if the manufacturer’s instructions are vague, they’ll guess. That’s why it’s critical to get your guidance directly from your prescriber or a trusted pharmacy. Don’t rely on memory, Google, or advice from a friend.
How to Avoid Missed Doses in the First Place
The best way to handle a missed dose? Don’t miss it.- Use a pill organizer with days of the week and morning/evening slots.
- Set alarms on your phone for each dose.
- Link taking your meds to a daily habit-like brushing your teeth or having breakfast.
- Use apps like MyTherapy or Medisafe. A 2023 study showed users reduced missed doses by 42.3%.
What to Do If You Already Took a Double Dose
If you accidentally took two doses:- Don’t panic-but don’t ignore it either.
- Call your pharmacist or GP immediately. If it’s after hours, contact NHS 111.
- Know your medication’s risk level. If it’s red-category (warfarin, insulin, etc.), seek help right away.
- Don’t take another dose until your next scheduled time.
When to Call for Help
You don’t need to wait for symptoms to get worse. Call your doctor or go to urgent care if you:- Took a double dose of a red-risk medication.
- Feel dizzy, nauseous, confused, or have unusual bleeding or bruising.
- Have chest pain, rapid heartbeat, or trouble breathing.
Final Rule: When in Doubt, Skip It
The safest default action after missing a dose is to skip it and wait for your next scheduled time. Doubling up is rarely the right move. Even if you feel fine, your body might not be. Medication safety isn’t about being perfect. It’s about being smart. One missed dose won’t ruin your treatment. But one double dose could change your life.Always check the specific instructions for your medication. When in doubt, ask your pharmacist. They’re trained to help you avoid harm-not just hand out pills.

Luke Davidson
January 24, 2026 AT 02:12Man I used to double up on my blood pressure meds all the time thinking it’d make me feel better faster. Turns out I was just setting myself up for a trip to the ER. This post saved my life honestly. Now I use Medisafe and it beeps at me like a loyal dog reminding me to take my pills. No more guesswork.
Also side note: my grandma took two warfarin pills once because she thought she missed one. Ended up in the hospital for a week. She’s fine now but she won’t touch her meds without checking the app first. We all learn the hard way.
Jenna Allison
January 26, 2026 AT 01:40As a pharmacist, I see this every single day. Patients Google ‘what if I miss a pill’ and get conflicting answers from blogs, Reddit, and YouTube influencers. The real issue? Most drug leaflets are written by lawyers, not clinicians. I tell my patients: if it’s not clearly spelled out, call us. We’re paid to answer this stuff.
Also-yes, some antibiotics like amoxicillin are safe to double up on. But 97% of people don’t know which ones. Always ask. No shame in it.
Phil Maxwell
January 27, 2026 AT 02:49Been on levothyroxine for 8 years. Always took it the second I remembered, even if it was 8 PM. Turns out the NHS updated their guidelines last year and I didn’t even know. Guess I’m guilty of trusting the old leaflet. This post was a wake-up call. I just reset my alarm to 7 AM. No more midnight thyroid pills.
Elizabeth Cannon
January 28, 2026 AT 07:39my man just took 2 of his glp-1 because he thought he missed it last week. he’s been puking for 2 days. i told him to call his doc but he said ‘nah im fine’ and now he’s texting me memes about ‘glp-1 warriors’. we need to talk about how nobody teaches you how to take your own meds like its common sense.
also why do pharms keep printing leaflets in 5pt font??
venkatesh karumanchi
January 28, 2026 AT 13:24In India, many people take insulin without proper guidance. I’ve seen patients skip doses for days, then take triple the dose on the 4th day because they’re scared of high sugar. It’s dangerous. This article is a lifeline. I’ve shared it with my family and my neighbor’s uncle who’s on warfarin. Knowledge should be free, not locked behind clinic visits.
Tommy Sandri
January 29, 2026 AT 12:26While the advice provided is generally sound, it’s worth noting that clinical guidelines vary internationally. The NHS recommendations referenced here are not universally adopted. In the U.S., for example, some institutions still advise taking missed once-daily doses within 24 hours, particularly for medications with long half-lives. This discrepancy underscores the need for patient-specific guidance rather than generalized protocols. The NPSA classification system, while useful, is not FDA-endorsed and may not align with U.S. pharmacy practice standards.
Darren Links
January 29, 2026 AT 16:21So let me get this straight - the government tells us not to double up on pills… but then they print instructions in tiny font that no one can read? And the pharmacies give conflicting advice? And you want us to trust ‘the system’? This is just another way they keep us dependent. I bet the drug companies profit when we end up in the hospital. They make more money off complications than they do off pills.
Next thing you know, they’ll tell us not to breathe too hard or we’ll overdose on oxygen. Wake up people.
Helen Leite
January 31, 2026 AT 09:42ALERT 🚨 THE PHARMA COMPANIES ARE LYING TO YOU!! 🚨
They don’t want you to know this but the ‘narrow therapeutic index’ thing? Total scam. The real reason you can’t double up is because they want you to keep buying more pills. They’re making billions off your confusion. I saw a video where a guy who took 2 warfarin pills and lived just fine. They covered it up.
Also, why do all the apps cost money? Free apps are government spyware. Use a paper calendar. They can’t track you there. 😈💊