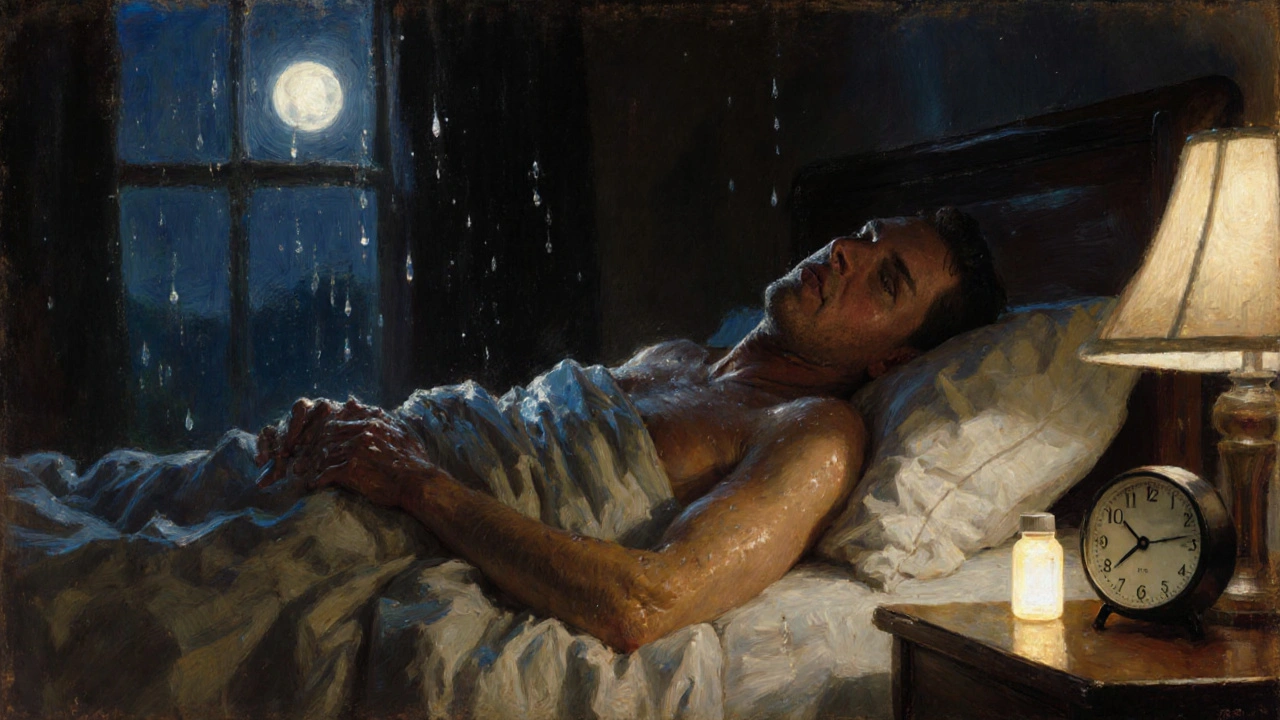
When you start taking an antidepressant, you expect relief from anxiety or depression-not to wake up soaked through in the middle of the night, or walk into a meeting with sweat dripping down your back. Yet excessive sweating from antidepressants is far more common than most people realize. Up to 22% of people on these medications report sweating so severe it disrupts sleep, ruins clothes, and makes social situations unbearable. This isn’t just discomfort-it’s a leading reason people quit their meds, even when they’re working. The good news? There are real, science-backed ways to manage it.
Why Antidepressants Make You Sweat
Antidepressant-induced excessive sweating, or ADIES, isn’t just "being hot." It’s a direct side effect of how these drugs interact with your brain’s temperature control system. Most antidepressants-especially SSRIs like sertraline and paroxetine-boost serotonin levels. But serotonin doesn’t just affect mood. It also talks to the hypothalamus, the part of your brain that regulates body temperature. When that signal gets scrambled, your body thinks it’s overheating… even when it’s not. This isn’t a rare glitch. A 2022 study in PMC9129361 found 7-19% of people on SSRIs experience noticeable sweating. Paroxetine tops the list at nearly 19%, while fluvoxamine is one of the lowest offenders at around 4%. SNRIs like venlafaxine and even bupropion (often chosen to avoid sexual side effects) carry similar risks. Tricyclics, though used less now, are also major culprits. The sweating usually starts within weeks, but sometimes creeps in after months of stable use. And here’s the kicker: tolerance rarely develops. If you’re sweating after three months, you’re probably still going to be sweating after three years.Which Antidepressants Cause the Most Sweating?
Not all antidepressants are created equal when it comes to sweating. Here’s what the data shows:| Medication | Class | Sweating Incidence | Notes |
|---|---|---|---|
| Paroxetine | SSRI | 19% | Highest risk; often causes severe sweating |
| Sertraline | SSRI | 14% | Commonly reported by users on forums |
| Escitalopram | SSRI | 12% | Can switch to citalopram for relief |
| Venlafaxine | SNRI | 11% | Immediate-release form worse than extended-release |
| Bupropion | NDRI | 10% | Lower sexual side effects, but similar sweating risk |
| Fluoxetine | SSRI | 7% | One of the lowest-risk SSRIs |
| Fluvoxamine | SSRI | 4% | Lowest sweating risk among SSRIs |
| Trazodone | SARI | 3% | Often used as alternative for those with sweating issues |
What’s surprising is how small changes can make a big difference. One case report in Psychiatric Times showed a patient switching from escitalopram to citalopram-same dose, same chemical family, but different molecular shape-had complete resolution of sweating. That’s because citalopram is the racemic mix, while escitalopram is just the active S-enantiomer. That tiny difference changes how it binds to serotonin receptors, and suddenly, your body doesn’t misread the signal.
When Sweating Is a Medical Emergency
Not all sweating is ADIES. If you’re sweating heavily and you have tremors, rapid heartbeat, confusion, high fever, or muscle rigidity, this could be serotonin syndrome-a rare but life-threatening reaction. It usually happens when you’ve recently increased your dose, added another medication, or combined antidepressants with supplements like St. John’s wort or certain painkillers. Serotonin syndrome needs immediate care. Don’t wait. Go to the ER. ADIES is annoying. Serotonin syndrome can kill you. If you’re unsure, err on the side of caution. The key difference? Sweating alone? Likely ADIES. Sweating plus shaking, racing heart, and fever? Emergency.
What Actually Works to Cool Down
There’s no one-size-fits-all fix, but these strategies have real evidence behind them:1. Switch Medications
This is the most effective long-term solution-if your depression is under control. Studies show switching from high-risk SSRIs like paroxetine or sertraline to fluvoxamine or trazodone often cuts sweating by 70% or more. Even switching from escitalopram to citalopram (same dose) has worked for people who had no luck with anything else. Don’t assume your doctor will bring this up. Many don’t realize how common and debilitating ADIES is. If you’re struggling, say it outright: “The sweating is making it impossible to keep taking this. Can we try something with lower risk?”2. Add an Anticholinergic
If switching meds isn’t an option, doctors can prescribe low-dose anticholinergics to block the sweat response. Two are most commonly used:- Glycopyrrolate: 1-2 mg daily. Reduces sweating in 70-80% of users. Side effects: dry mouth, constipation, blurred vision. Usually well-tolerated at low doses.
- Benztropine: 0.5-1 mg daily. Also helps with tremors if present. Used more often in older patients.
3. Try Terazosin
This is a blood pressure medication, but it’s also an alpha-blocker that can reduce sweating. A 2022 study found 5 mg of terazosin at night reduced sweating by 60-70% in patients who didn’t respond to other options. It’s not FDA-approved for this use, but it’s used off-label with good results. Side effects: dizziness, especially when standing up. Start low-1 mg at night-and increase slowly.4. Use Cooling Gear
You can’t always change your meds. But you can change your clothes and environment.- Cooling vests: A 2022 pilot study found 60% of users reported significant relief. These vests use phase-change materials that absorb heat and stay cool for hours.
- Miracle-wicking fabrics: Look for moisture-wicking underwear and shirts made from polyester blends or merino wool. Cotton holds sweat. These fabrics pull it away and dry fast.
- Antiperspirants with 15-20% aluminum chloride: Apply at night to underarms, chest, or even scalp (yes, scalp). This isn’t your drugstore brand-it’s clinical strength. Brands like Drysol or Certain Dri work. You might feel tingling at first. That’s normal.
5. Environmental Tweaks
Simple changes make a big difference:- Keep your bedroom at 65-67°F (18-19°C). Use a fan or air conditioner.
- Take a cool shower before bed.
- Avoid caffeine, alcohol, and spicy food in the evening-they raise body temperature.
- Wear loose, layered clothing so you can peel off layers if you start to sweat.
What Doesn’t Work (and Why)
A lot of advice you hear online is wrong:- Reducing your antidepressant dose: Only helps about 40% of the time-and if your depression is improving, lowering the dose can make it worse.
- Herbal remedies like sage or witch hazel: No solid evidence they work for medication-induced sweating.
- Just “getting used to it”: As noted in the 2000 Pierre and Guze study, tolerance rarely develops. This isn’t something you grow out of.


Denny Sucipto
November 17, 2025 AT 13:11Been there. Took sertraline for 8 months, woke up like I’d been in a sauna. Switched to fluoxetine and it’s like night and day. No more soaked shirts at work. Seriously, if you’re sweating buckets, don’t just suffer-talk to your doc about swapping meds. It’s not weakness, it’s science.
Bailey Sheppard
November 18, 2025 AT 11:08Thank you for writing this. So many people think it’s just ‘being hot’ or ‘not trying hard enough.’ This is legit medical stuff. I’ve been on trazodone for a year now-barely sweat at all. And yeah, cooling vests? Game changer. I wear one under my blazer to meetings. No one knows, but I’m dry as a bone.
steffi walsh
November 18, 2025 AT 15:03Yessss!!! This is the post I needed last year 😭 I was on paroxetine and I cried in the shower because my hair was dripping and I had to change clothes 3x a day. Switched to fluvoxamine and now I sleep through the night. You’re not alone. 💪❤️
Riohlo (Or Rio) Marie
November 19, 2025 AT 01:35How quaint. You all treat this like some minor inconvenience, but let’s be real-this is a pharmacological betrayal. SSRIs are designed to hijack your neurochemistry, and sweating is the least of your worries. The real issue? The pharmaceutical-industrial complex doesn’t want you to know that 19% of users get drenched because they’re prioritizing profit over precision. You’re not broken-you’re being exploited. And no, glycopyrrolate won’t fix the system.
Holly Powell
November 19, 2025 AT 02:32While the clinical data presented is superficially compelling, it lacks longitudinal biomarker correlation. The assumption that serotonin receptor binding affinity directly correlates with sudomotor dysfunction is reductionist at best. One must account for polymorphic CYP2D6 phenotypes, which modulate metabolite accumulation and thus peripheral serotonergic tone. Without pharmacokinetic stratification, these incidence rates are statistically noise.
Yash Nair
November 19, 2025 AT 18:45uS people always overcomplicate everything. In India we just use alum stone. Rub it on armpits before bed. Done. No pills. No vests. No drama. Your body will adjust if you stop whining. Also, why are you taking antidepressants anyway? Life is hard everywhere. Just be strong.
Conor McNamara
November 21, 2025 AT 00:16you ever think the sweat isnt from the drug… but from the gov’t microchips in the pills? i read a guy on 4chan who said the 2022 study was faked by big pharma to distract from the real issue: the 5g towers in your city are syncing with your sweat glands. i switched to fluvoxamine and the sweating got worse. coincidence? i think not.
Emanuel Jalba
November 22, 2025 AT 21:42THIS IS WHY WE CAN’T HAVE NICE THINGS 😭 I was on sertraline and I had to wear a towel under my shirt to work. My boss thought I was a mess. My girlfriend left me because she said I smelled like a gym locker. I cried so hard I woke up my cat. I’m not okay. Someone please help me. 🥺
Kristi Joy
November 24, 2025 AT 19:16Hey everyone-just wanted to say thank you for sharing. This is the kind of real talk that saves lives. If you’re reading this and you’re sweating through your life, please know: you’re not failing. You’re adapting. And there are options. Talk to your doctor. Bring this article. You deserve to feel comfortable in your own skin.
Hal Nicholas
November 26, 2025 AT 06:58Let’s be honest-this whole thread is just a pity party for people who can’t handle basic discomfort. If you’re sweating because of a pill, maybe you shouldn’t be on it. People in the 1950s didn’t have cooling vests and anticholinergics. They just dealt with it. Maybe your depression isn’t that severe after all.
Louie Amour
November 27, 2025 AT 02:30Wow. You people are so naive. You think switching meds is the answer? You think glycopyrrolate fixes anything? No. The real problem is that you’re all too emotionally dependent on pharmaceuticals. You need to do yoga, eat turmeric, and reconnect with your ancestral roots. This isn’t a medical issue-it’s a spiritual failure.
Leilani O'Neill
November 29, 2025 AT 00:24As an Irishwoman who’s seen this nonsense for decades, I’m appalled. You Americans treat mental health like a Walmart product. ‘Oh, I sweat too much? Just swap pills!’ No. We don’t need more options-we need better discipline. Back in Cork, we’d just put on a wool sweater and walk to the sea. Cold water. Fresh air. No magic vests. No chemicals. Just grit.
Girish Pai
November 29, 2025 AT 01:55Bro, you're all missing the point. In India, we have a solution called 'khus khus'-it's a cooling herb. You soak it in water, drink it, and your body temp drops. No side effects. No pills. Just pure ayurveda. Why are you wasting money on terazosin and cooling vests? You're not trying hard enough. This is why the West is falling behind.