Pregnancy Test Accuracy Calculator
Results will appear here
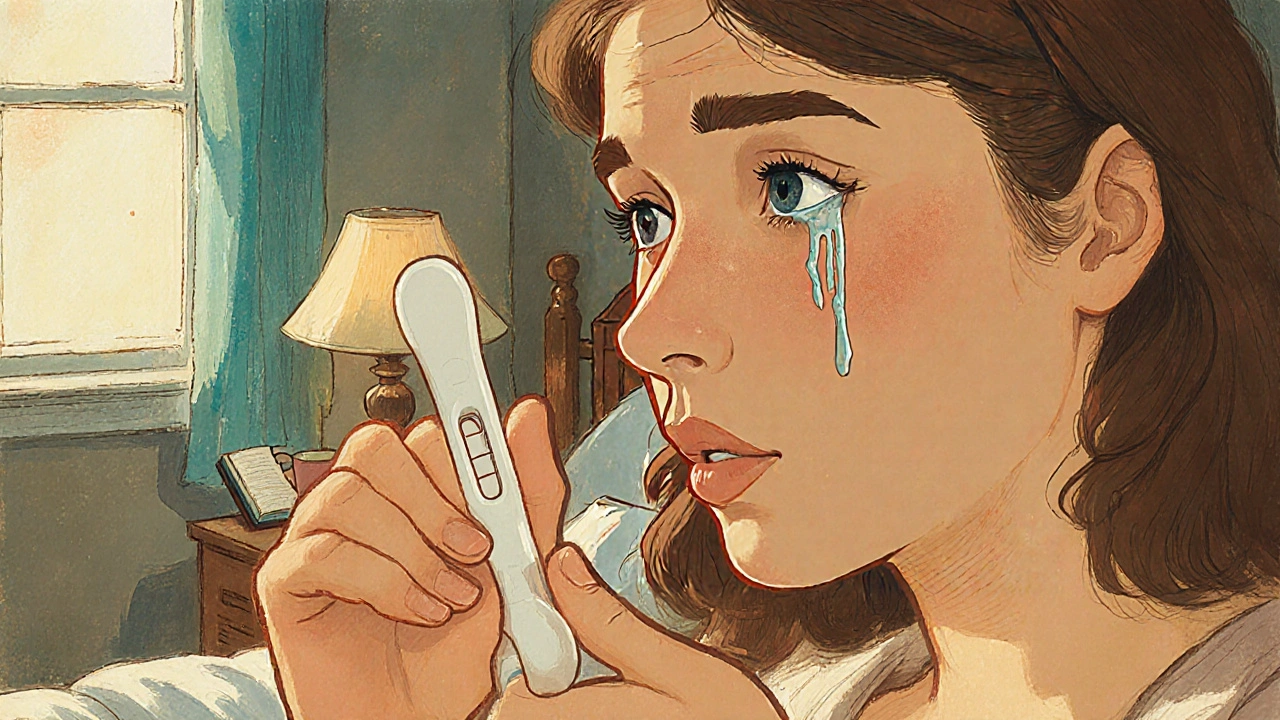
Finding a negative pregnancy test when you hoped for a different answer can feel like an emotional roller‑coaster. You might be confused, disappointed, or even scared. The good news is that you’re not alone, and there are clear, doable steps you can take to understand what the result means and to look after yourself.
What a negative pregnancy test result actually tells you
Most home tests use a strip that detects Human chorionic gonadotropin (hCG), the hormone your body starts making after a fertilized egg implants. If the strip doesn’t pick up enough hCG, it shows a negative line. That usually means either you’re not pregnant, the test was taken too early, or the urine was too diluted.
Pregnancy test strips are designed to be 99% accurate when used correctly. The key is timing - testing after a missed period gives the most reliable reading. If you tested early, the hormone might not have built up enough to be detected.
Why your emotions might feel intense
Our bodies are wired to react strongly to hopes and fears, especially around something as life‑changing as pregnancy. The hormone Stress can amplify feelings of anxiety, sadness, or frustration. It’s normal to wonder, “Did I do something wrong?” or “What does this mean for my future?” Acknowledge those thoughts instead of pushing them away - they’re a sign your mind is processing the news.
Talk to a trusted friend or partner if you can. Simply voicing what’s on your mind can lower the emotional load. If you feel stuck, consider a quick journal entry: write down what you’re feeling, any physical sensations, and what you hope to do next. Seeing it on paper often brings clarity.
Immediate practical steps after a negative result
- Re‑check the test instructions. Make sure you waited the recommended time before reading the result.
- If you tested before your missed period, wait a few days and test again. Ovulation timing can shift, affecting hormone levels.
- Stay hydrated but avoid overly diluted urine - a mid‑morning sample works best.
- Track your cycle in a calendar or app. Note any symptoms like breast tenderness or mild cramping; they can help you pinpoint future fertile windows.
- Consider a follow‑up appointment with a Healthcare professional if you’ve had multiple negative results but still suspect pregnancy.
Long‑term coping strategies
Whether you’re planning to try again, dealing with an unexpected outcome, or simply need time to process, these strategies can keep you grounded.
- Emotional support: Join a local Support group for people navigating similar experiences. Many groups meet in Melbourne community centres or run online via video chat.
- Mind‑body practices: Gentle yoga, meditation, or even a daily walk can lower cortisol, the stress hormone, and improve mood.
- Nutrition and Lifestyle changes: Balanced meals with plenty of fruits, vegetables, and protein support overall health and hormone balance.
- Education: Learn about your Fertility cycle. Understanding the science behind Early pregnancy symptoms versus pre‑menstrual signs can reduce uncertainty.
- Professional counselling: If feelings of loss, disappointment, or anxiety linger for weeks, a psychologist specializing in reproductive health can offer tools to cope.
When to seek medical advice
If you notice any of the following, schedule a visit with your doctor promptly:
- Persistent pelvic pain or heavy bleeding.
- Signs of a possible ectopic pregnancy (sharp pain on one side, faintness).
- Repeated negative home tests despite missed periods.
- Underlying health conditions (PCOS, thyroid issues) that could affect hormone readings.
Your doctor may order a blood test to measure hCG levels more precisely, or an ultrasound if they suspect an early pregnancy or other concerns.

Comparison of coping strategies
| Strategy | When to use | Typical duration | Example actions |
|---|---|---|---|
| Re‑test and verify | Within 48‑72 hours of first result | 1‑2 days | Follow test instructions, use mid‑morning urine |
| Talk to a friend or partner | Immediately after result | As needed | Phone call, coffee meet‑up, video chat |
| Join a support group | Within the first week | Ongoing | Attend weekly Melbourne meet‑up, online forum |
| Professional counselling | If emotions stay intense after 2 weeks | Several sessions | Book a reproductive psychologist |
| Medical consultation | Any alarming physical symptoms | One appointment, possibly follow‑up | Blood hCG test, ultrasound |
Quick checklist for the next 48 hours
- Review test instructions for timing and urine concentration.
- Log your last menstrual period and any symptoms.
- Reach out to a trusted person for a quick chat.
- Plan a second test for the next morning if you tested early.
- Note any physical discomfort - schedule a doctor’s visit if needed.
How soon after a missed period should I take a home pregnancy test?
Most tests are reliable from the first day of a missed period. Waiting 24‑48 hours can improve accuracy, especially with early‑detection kits.
Can a negative result be a false negative?
Yes. Testing too early, using diluted urine, or a faulty test can lead to a false negative. Re‑testing a few days later helps rule this out.
Should I see a doctor after a negative test if I still feel pregnant?
If you have persistent symptoms like breast tenderness, nausea, or missed periods, a blood hCG test can provide a definitive answer. Your GP or a reproductive health clinic can arrange this.
What emotional resources are available in Melbourne?
The Victorian Family Planning Council runs free support groups, and many community health centres offer counselling specifically for reproductive concerns.
Can lifestyle changes improve my chances for a future pregnancy?
Eating a balanced diet, maintaining a healthy weight, limiting alcohol, and managing stress are all proven to boost fertility. Regular exercise and quitting smoking also help.

DHARMENDER BHATHAVAR
October 19, 2025 AT 14:59While a negative result can feel disappointing, it also provides an opportunity to reassess timing and health habits. Review the test instructions, ensure you used a mid‑morning sample, and consider logging your cycle in an app. This systematic approach will give you clearer insight for your next attempt.
Kevin Sheehan
October 19, 2025 AT 15:20It is absurd to let a single strip dictate the narrative of your future; the universe operates beyond our immediate perception. If you let anxiety dominate, you surrender agency. Instead, confront the uncertainty head‑on, recalibrate expectations, and recognize the test as merely one data point in a larger continuum of possibilities.
Jay Kay
October 19, 2025 AT 16:43Honestly, the article regurgitates the same checklist you've seen a hundred times on every health blog. There's nothing groundbreaking here-just generic advice wrapped in a soothing tone. If you're looking for real insight, you need more than a bullet‑point list; you need personal accountability.
Penny Reeves
October 19, 2025 AT 18:06It is commendable that the guide emphasizes both the physiological and emotional aspects of receiving a negative pregnancy test. First, understanding the biochemical mechanism of hCG detection demystifies the process and reduces misplaced blame. Second, acknowledging the emotional turbulence validates the lived experience of many individuals. However, the article could benefit from a deeper exploration of the psychological aftermath beyond a simple suggestion to “talk to a friend.” Long‑term coping mechanisms such as cognitive‑behavioral strategies and structured journaling have been shown to alleviate ruminative thoughts. Additionally, the recommendation to join a support group in Melbourne is geographically narrow; virtual communities can provide equal, if not greater, accessibility. Nutrition advice, while useful, should be contextualized with evidence‑based guidelines rather than generic statements. The checklist format, while handy, risks oversimplifying complex emotional states into tick‑boxes. Readers would appreciate a nuanced discussion of how cultural expectations shape reactions to negative results. Moreover, the role of the partner in the coping process deserves more attention, as shared decision‑making often mitigates feelings of isolation. The article briefly mentions medical consultation but does not elaborate on the diagnostic value of serum hCG versus urine tests. Clarifying this distinction can empower readers to make informed choices. A brief overview of common hormonal disorders such as PCOS and their impact on test accuracy would also be valuable. The inclusion of a table comparing immediate and long‑term strategies is visually effective, yet the table lacks citations to reputable sources. Finally, integrating personal anecdotes or case studies could humanize the content and foster deeper engagement. Overall, the guide is a solid foundation, but with these enhancements it could evolve into a comprehensive resource for anyone navigating this challenging period.
Sunil Yathakula
October 19, 2025 AT 19:30Hey, i totally get how you feel rn. It’s normal to be sad after a negative test, but dont forget you’ve got options. Try re‑testing in a few days, keep a hydration schedule, and maybe chat with a friend about it. Small steps can make a big diff. Keep your head up, mate.
dennis turcios
October 19, 2025 AT 20:53The article correctly outlines the physiological basis of hCG detection, yet it glosses over the statistical false‑negative rate in early testing. Peer‑reviewed studies suggest that up to 5 % of early tests may miss a viable pregnancy. Moreover, the recommendation to “stay hydrated” lacks nuance; excessive fluid intake can dilute urine, potentially leading to erroneous results. A more detailed discussion of test sensitivity thresholds would strengthen the piece.
Felix Chan
October 19, 2025 AT 22:16Great reminder to stay patient and keep hope alive!
Thokchom Imosana
October 19, 2025 AT 23:40Consider how the pharmaceutical industry capitalizes on our anxieties about fertility, pushing us toward incessant testing without addressing underlying societal pressures. The narrative that a single negative strip is a definitive endpoint obscures the broader context of reproductive surveillance. Many health platforms subtly steer users toward costly clinics, perpetuating a cycle of dependency. While the guide offers practical steps, it fails to question why we accept this paradigm without critique. Awareness of these dynamics can empower individuals to seek holistic well‑being beyond the confines of a test strip.
ashanti barrett
October 20, 2025 AT 01:03I hear you, and it’s vital to acknowledge those feelings without letting them fester. Sharing your experience with a trusted confidant can transform uncertainty into actionable steps. Don’t shy away from seeking professional guidance if anxiety persists; mental health is just as important as physical health.
Leo Chan
October 20, 2025 AT 02:26Remember, every cycle teaches you something new about your body. Celebrate the small victories-like tracking your basal temperature or noting cervical mucus changes. Those details will empower you when you decide to try again.
jagdish soni
October 20, 2025 AT 03:50In the grand tapestry of human reproduction the negative strip is but a fleeting whisper a momentary silence that beckons introspection It is through such silences that the soul contemplates the architecture of desire and destiny One must not merely consume the checklist but rather meditate upon the existential weight of longing and the societal narratives that dictate our notions of success and failure In this light the article serves as a mirror reflecting our collective anxieties while also offering a pragmatic scaffold upon which we may rebuild our hopes