When your prescription runs out and the pharmacy can’t restock
You’ve been taking the same medication for months - maybe years. Then one day, your pharmacy says, "It’s out of stock. We don’t know when it’ll be back." This isn’t rare. In 2025, the U.S. saw over 350 drug shortages, affecting everything from antibiotics to blood pressure pills. For many people, this isn’t just an inconvenience - it’s a health crisis.
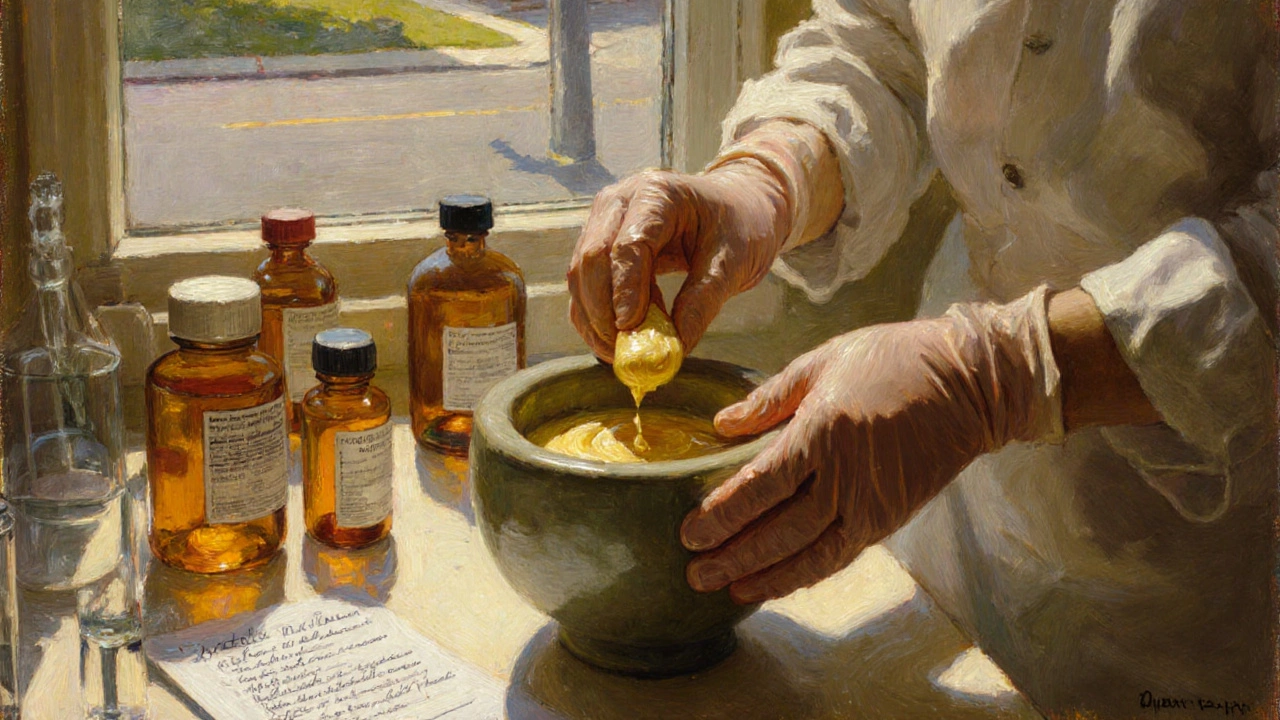
That’s where compounding pharmacies come in. They don’t just fill prescriptions. They build them from scratch when nothing else works.
What exactly is a compounding pharmacy?
Most pharmacies hand out pills made by big drug companies. Compounding pharmacies are different. They’re like medical labs run by pharmacists. Instead of pulling a pre-made tablet off a shelf, they mix raw ingredients to create exactly what your body needs.
Think of it like baking a cake when you’re out of flour. You don’t stop eating - you use what you have. Compounding pharmacists do the same with medicine. They can make:
- Liquids instead of pills for kids or seniors who can’t swallow
- Topical creams for pain or hormone therapy
- Doses that aren’t sold commercially - like 5mg instead of 10mg or 25mg
- Formulas without dyes, gluten, lactose, or preservatives if you’re allergic
This isn’t science fiction. It’s standard practice. About 7,500 pharmacies in the U.S. specialize in this. And over 32,000 offer some level of compounding. These aren’t fringe operations - they’re a lifeline.
Why do drug shortages happen so often?
Drug shortages aren’t random. They’re caused by a mix of supply chain problems, manufacturing delays, and single-source production. A lot of medications are made in just one or two factories. If one shuts down for inspections, or a raw material gets stuck at customs, the whole country runs out.
Some of the most common shortages in 2025 include:
- Levothyroxine (for thyroid)
- Amoxicillin (antibiotic)
- Insulin (for diabetes)
- Propranolol (for heart and migraines)
When these go missing, patients are left with no clear path forward. That’s where compounding pharmacies step in. They can replicate the active ingredient and deliver it in a different form - often within 24 to 72 hours.
Who benefits the most from compounded medications?
It’s not just about shortages. Compounding helps people who can’t use regular drugs - even when they’re available.
Children: About 40% of kids struggle with swallowing pills. A compounded cherry-flavored liquid version of a medication can turn a daily struggle into a routine.
Elderly patients: One in three seniors has trouble swallowing. Compounding turns pills into gels you rub on your skin or liquids you sip.
Allergy sufferers: Around 15-20% of people react to dyes, gluten, or preservatives in pills. A compounded version removes those triggers. One study showed 85% better adherence when patients got allergen-free versions.
Chronic pain or hormone therapy patients: Compounding allows precise dosing - like 2mg of testosterone gel daily instead of a 10mg patch that causes side effects. Hormone therapy makes up nearly 30% of all compounded prescriptions.
How does the process work?
It’s not as simple as walking in and asking for a custom pill. Here’s how it actually works:
- Your doctor identifies that your current medication isn’t working - either because it’s unavailable or causes side effects.
- Your doctor writes a prescription for a compounded version, including exact strength, form, and ingredients.
- You take that prescription to a compounding pharmacy (some pharmacies offer both services; others specialize).
- The pharmacist reviews the formula, checks safety, and prepares your medication in a clean room.
- You pick it up in 1-3 days.
It’s not instant. But it’s reliable. And it’s backed by strict rules. Compounding pharmacies follow USP <795> for non-sterile mixes and USP <797> for sterile ones - meaning they work in controlled environments with special equipment.
How do you know if a compounding pharmacy is legit?
Not all pharmacies that say they compound are created equal. The biggest red flag? No accreditation.
Look for the Pharmacy Compounding Accreditation Board (PCAB) seal. Only about 1,200 of the 7,500 compounding pharmacies in the U.S. have this. PCAB accreditation means they’ve passed inspections for cleanliness, training, and quality control.
Ask these questions:
- "Are you PCAB-accredited?"
- "Do you test your batches for potency and purity?"
- "Can I see your stability data for this medication?"
Reputable pharmacies will have this info ready. If they hesitate, walk away.
What can’t compounding pharmacies do?
They’re powerful - but not magic. There are limits:
- They can’t make biologics (like insulin from genetically modified bacteria)
- They can’t replicate complex IV drugs that require sterile manufacturing lines
- They can’t replace FDA-approved drugs when those drugs are available and safe
Some doctors overprescribe compounded meds when a regular pill would work. That’s risky. Compounded drugs don’t go through the same pre-market testing as brand-name drugs. They’re safe - but only when used correctly.
As one pharmacist put it: "We’re not here to replace the system. We’re here to fix the gaps."
Cost and insurance: What to expect
Here’s the tough part: insurance doesn’t always cover compounded meds.
About 45% of patients pay out-of-pocket. That’s because insurers don’t have standard codes for custom formulas. Some will cover it if your doctor writes a letter of medical necessity. Others won’t touch it.
Costs vary. A compounded cream might be $40-$80. A liquid suspension could be $60-$120. Compare that to a $10 generic pill - it’s more expensive. But for many, it’s the only option.
GoodRx and other price-comparison tools now list some compounded meds. Call ahead. Ask for a cash price. Some pharmacies offer discounts for long-term prescriptions.

Real stories: Why people swear by compounding
One Reddit user shared how his 12-year-old son couldn’t take oral ADHD meds due to nausea. The compounding pharmacy made a transdermal gel. Within a week, his son was focused in school - and no longer vomiting.
A 68-year-old woman with severe arthritis couldn’t swallow pain pills. Her pharmacist made a topical cream with ketoprofen and lidocaine. She stopped using opioids.
A man with a rare allergy to dyes in his blood pressure med had daily migraines. His compounding pharmacist removed the dye and switched him to a capsule with a different binder. His headaches vanished.
These aren’t outliers. They’re everyday cases. And they’re why 89% of patients who use compounded meds say they’d recommend them to others.
What’s changing in 2025?
The FDA updated its guidance in late 2024, making it clearer when compounding is allowed during shortages. More pharmacies are investing in digital tools that cut compounding errors by 37%. Stability testing now extends shelf life by up to 40% - meaning less waste and fewer repeat visits.
There’s also a push toward personalized medicine. Pharmacists are starting to use genetic test results to tailor dosing - especially for antidepressants and blood thinners. That’s the future: not one-size-fits-all, but one-size-fits-you.
What to do next if your drug is unavailable
If you’re stuck with a shortage:
- Don’t skip doses. Talk to your doctor immediately.
- Ask: "Can we switch to a compounded version?"
- Find a PCAB-accredited compounding pharmacy near you. Use the IACP directory (International Academy of Compounding Pharmacists).
- Get a written prescription with exact specs - strength, form, ingredients.
- Call ahead. Ask about turnaround time and cost.
- Follow up. Check that your medication works as expected.
Compounding isn’t a first resort. But when everything else fails, it’s the best second one.
Are compounded medications safe?
Yes - when made by accredited pharmacies following USP standards. Compounded drugs don’t go through the same FDA approval process as mass-produced drugs, but they’re held to strict quality and cleanliness rules. Always choose a PCAB-accredited pharmacy to ensure safety.
Can I get compounded meds without a prescription?
No. Compounded medications require a valid prescription from a licensed provider. Pharmacists cannot create custom formulas without a doctor’s order. This is required by law to protect patient safety.
How long does it take to get a compounded prescription?
Most take 24 to 72 hours to prepare. Sterile compounds - like injections or IV solutions - can take longer due to additional testing. Non-sterile formulas like creams or liquids are usually ready faster. Always ask your pharmacy for an estimated pickup time.
Does insurance cover compounded medications?
Sometimes. About 55% of patients pay out-of-pocket because insurers don’t have standard codes for custom formulas. You can increase your chances by having your doctor write a letter of medical necessity. Some pharmacies offer cash discounts or payment plans.
What’s the difference between 503A and 503B compounding pharmacies?
503A pharmacies are smaller, community-based labs that make prescriptions for individual patients. 503B outsourcing facilities are larger, FDA-registered operations that can produce in bulk for clinics and hospitals. Most patients use 503A pharmacies. 503B is for large-scale shortages, not personal prescriptions.
Final thought: You’re not alone
Drug shortages feel isolating. But you’re not the only one stuck. Thousands of people rely on compounding pharmacies every day. These aren’t backup plans - they’re essential tools in modern medicine. If your medication disappears, don’t panic. Talk to your doctor. Find a qualified compounding pharmacy. And know that there’s a way forward - even when the shelves are empty.


Jeremy Samuel
November 21, 2025 AT 04:11Destiny Annamaria
November 22, 2025 AT 15:55Ron and Gill Day
November 23, 2025 AT 14:12Alyssa Torres
November 25, 2025 AT 10:52Summer Joy
November 27, 2025 AT 10:01Shiv Karan Singh
November 27, 2025 AT 16:24Ravi boy
November 29, 2025 AT 11:10Matthew Karrs
November 30, 2025 AT 17:07Matthew Peters
December 1, 2025 AT 14:32