Chlorambucil Dose Calculator for Pediatric Patients
Dosage Calculator
Calculate the appropriate chlorambucil dosage for pediatric patients based on body surface area (BSA). This tool uses the Mosteller formula for BSA calculation and provides standard dosing ranges for different pediatric cancer scenarios.
When doctors face a child's cancer, they often turn to drugs that can halt DNA replication. Chlorambucil is an oral alkylating agent that has been used for decades in adult leukemias and, increasingly, in certain pediatric protocols. In Pediatric Oncology, its role is niche but critical, especially when the disease is resistant to first‑line therapy.
Chlorambucil remains a valuable option in the pediatric arsenal because it can be given by mouth, sparing young patients from frequent IV lines. This article breaks down what the drug does, which childhood cancers it touches, how doctors dose it safely, and what families should watch for during treatment.
What Is Chlorambucil?
Chlorambucil belongs to the class of alkylating agents. Its chemical name is 4‑[4‑(dimethylamino) phenyl]‑2,6‑dichloro‑1,3,5‑triazine. In plain language, it adds a small chemical “alkyl” group to the DNA strands of rapidly dividing cells. This creates cross‑links that prevent the DNA from uncoiling, effectively stopping the cancer cells from multiplying.
- Mechanism of action: DNA cross‑linking → replication block → cell death.
- Administration: Oral tablets, typically 2 mg or 4 mg.
- History: Approved in the United States in 1957 for chronic lymphocytic leukemia; later explored for other hematologic malignancies.
Why Consider Chloralkylating Agents in Children?
Children’s bodies handle drugs differently than adults. Their liver enzymes and kidneys are still maturing, which can affect both efficacy and toxicity. Alkylating agents like chlorambucil have a few advantages that matter in a pediatric setting:
- Oral delivery: Reduces the need for central venous catheters, lowering infection risk.
- Long‑term experience: Decades of data help clinicians predict side‑effects and manage them proactively.
- Synergy with other drugs: Often combined with steroids, antimetabolites, or newer targeted therapies to boost response rates.
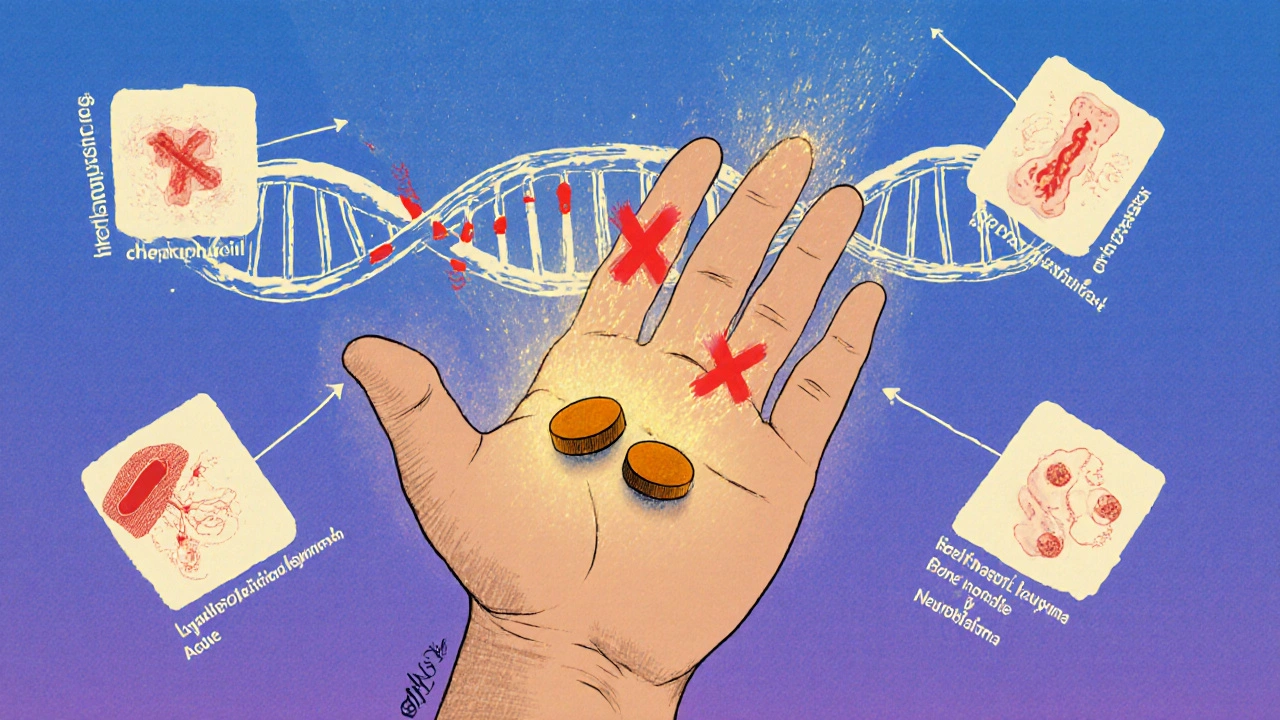
Childhood Cancers Where Chlorambucil Finds Use
Chlorambucil is not a first‑line cure for most pediatric cancers, but several scenarios call for its inclusion:
| Cancer Type | Typical Setting for Use | Usual Dose (mg/m²/day) | Key Side Effects |
|---|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) - relapsed | Combination rescue protocol | 0.2‑0.4 | Myelosuppression, nausea |
| Hodgkin Lymphoma - refractory | After failure of ABVD | 0.3 | Hair loss, mild liver enzyme rise |
| Juvenile Myelomonocytic Leukemia | Low‑intensity maintenance | 0.15‑0.25 | Infections, platelet drop |
| Neuroblastoma - high‑risk, salvage | Combined with cyclophosphamide | 0.2‑0.35 | Renal toxicity, mucositis |
These doses are given on a 1‑to‑3‑day schedule, often repeated every 3‑4 weeks depending on blood count recovery.
Dosing and Pharmacokinetics in Kids
Because children vary widely in size, the dose is calculated per square meter of body surface area (mg/m²). Pharmacokinetic studies from the early 2000s show:
- Absorption: Approximately 90 % oral bio‑availability.
- Distribution: Widely distributed; modest protein binding (~30 %).
- Metabolism: Primarily hepatic via CYP2C9; children often metabolize faster, so dose adjustments may be needed.
- Elimination: Renal excretion of unchanged drug and metabolites; clearance correlates with glomerular filtration rate.
Therapeutic drug monitoring is not routine, but clinicians may order plasma levels in cases of renal insufficiency or unexpected toxicity.
Managing Side Effects - What Families Should Know
Alkylating agents have a well‑known side‑effect profile. The most common issues in pediatric patients include:
- Myelosuppression: Low white blood cells, red cells, and platelets. Regular CBC checks (once a week) help catch drops early.
- Nausea & vomiting: Anti‑emetics like ondansetron are given prophylactically.
- Hair loss: Usually mild; children often experience thinning rather than complete baldness.
- Renal toxicity: More likely at higher cumulative doses. Hydration and periodic serum creatinine tests are standard.
- Secondary malignancies: Long‑term risk exists, especially with cumulative alkylator exposure. Survivorship clinics monitor for this over years.
Parents should keep a symptom diary, noting fevers, bleeding, or any new rash, and contact the oncology team right away.
Practical Tips for Caregivers
Even with a familiar drug like chlorambucil, the home environment can influence outcomes:
- Adherence: Set a daily alarm; tablets are usually taken with food to reduce stomach upset.
- Storage: Keep tablets at room temperature, away from moisture and out of reach of younger siblings.
- Vaccinations: Live vaccines are usually paused while the child’s blood counts are low.
- School considerations: Inform teachers about possible infection risk; arrange for a temporary leave if neutropenia is severe.
Future Directions - Is Chlorambucil Still Relevant?
New targeted therapies and immunotherapies dominate headlines, yet chlorambucil still shows up in clinical trials. Researchers are pairing it with:
- PARP inhibitors: The DNA‑damage synergy may improve response in refractory ALL.
- Low‑dose metronomic schedules: Continuous, low‑dose administration aims to curb angiogenesis while limiting toxicity.
- CAR‑T cell bridging: Using chlorambucil to reduce tumor burden before a CAR‑T infusion.
These studies suggest the drug will stay on the pediatric oncology toolbox for at least another decade, especially in low‑resource settings where oral chemotherapy is a logistical advantage.
Key Takeaways
- Chlorambucil is an oral alkylating agent that creates DNA cross‑links, stopping cancer cell growth.
- In children, it is mainly used for relapsed or refractory leukemias and lymphomas.
- Dosing is weight‑based (mg/m²) and requires close blood‑count monitoring.
- Common side effects include myelosuppression, nausea, and mild renal effects; long‑term risk of secondary cancers exists.
- Adherence, hydration, and vigilant infection monitoring are essential for safe use.
Can chlorambucil be used as a first‑line treatment for childhood leukemia?
No. Current protocols favor combination regimens that include vincristine, steroids, and asparaginase. Chlorambucil is typically reserved for relapsed or refractory cases where standard drugs have failed.
How is the dose of chlorambucil calculated for a child?
Doctors use body‑surface area (BSA) in mg per square meter. A typical maintenance dose ranges from 0.15 to 0.4 mg/m² per day, given for 1‑3 consecutive days every 3‑4 weeks, depending on blood count recovery.
What monitoring tests are required during treatment?
Weekly complete blood counts (CBC) are standard. Liver function tests and serum creatinine are checked every 2‑3 weeks. If the child shows signs of infection, a full septic work‑up is performed immediately.
Are there long‑term risks associated with chlorambucil?
Yes. Like other alkylating agents, chlorambucil carries a small but measurable risk of secondary cancers, especially after high cumulative doses. Survivorship programs schedule periodic screenings to catch any early signs.
Can chlorambucil be taken at home?
Yes. One of its main advantages is oral administration, which allows families to give the medication at home under the guidance of the oncology team. Proper storage and adherence are crucial.

Benedict Posadas
October 22, 2025 AT 19:42Yo fam! 🎉 Chlorambucil is a game‑changer for kids who hate needles – taking a pill at home beats a whole line of IVs any day. It’s definetly easier on the whole fam and cuts down infection risk bigtime. Keep that med in a dry place and set a daily alarm son you dont miss a dose! 😎
Jai Reed
November 1, 2025 AT 13:26It is essential to understand that chlorambucil dosing must be calculated precisely per square meter; any deviation can increase toxicity dramatically. Clinicians should monitor CBCs weekly and adjust doses without hesitation. The drug’s role is supplemental, not primary, and must be integrated into established protocols.
WILLIS jotrin
November 11, 2025 AT 09:33Thinking about the bigger picture, oral agents like chlorambucil shift part of the treatment burden from hospital to home, letting families maintain a sense of normalcy during tough cycles. Still, the psychological weight of daily meds can be heavy, so support networks are crucial.
Joanne Ponnappa
November 21, 2025 AT 05:40Appreciate the clear breakdown of dosing and side‑effects – really helps parents navigate the process. 😊 Keeping a symptom diary as suggested can catch issues early and avoid hospital trips.
Emily Collins
December 1, 2025 AT 01:46The shadow of secondary malignancies looms like a silent storm over every dose.
Harini Prakash
December 10, 2025 AT 21:53Remember, staying well‑hydrated and following the anti‑emetic schedule can make the treatment smoother 😊. If your child feels off, reach out – early intervention prevents bigger problems.
Rachael Turner
December 20, 2025 AT 18:00Life with cancer is a mosaic of moments each one fragile yet shining the way a sunrise splits the night the science of chlorambucil offers a thread through the chaos each dose is a step forward toward hope yet the side effects whisper reminders of the battle within the body we must listen keenly and respond with care
Vin Alls
December 30, 2025 AT 14:06Chlorambucil may sound like an old‑timer, but its utility in pediatric oncology is anything but antiquated. First, the oral route eliminates the logistical nightmare of placing a central line in a small child, which is a monumental relief for both nurses and parents. Second, the drug’s pharmacokinetics-high oral bioavailability, modest protein binding, and hepatic metabolism via CYP2C9-lend themselves to predictable dosing schedules. Third, when paired with steroids or modern targeted agents, chlorambucil can act as a silent partner, amplifying DNA damage beyond what any single agent could achieve alone. Fourth, the side‑effect profile, while not trivial, is well‑charted; myelosuppression, nausea, and mild renal effects are manageable with routine labs and supportive care. Fifth, long‑term surveillance for secondary malignancies, though a daunting prospect, has been mitigated by staggered dosing and cumulative dose caps established over decades of experience. Sixth, in low‑resource settings where infusion pumps are scarce, an oral tablet is a lifeline that keeps treatment on track. Seventh, the drug’s affordability compared to newer biologics ensures broader access across socioeconomic strata. Eighth, recent trials exploring low‑dose metronomic schedules suggest a new horizon where chlorambucil can double as an anti‑angiogenic agent. Ninth, the synergy observed with PARP inhibitors is sparking excitement in labs studying refractory ALL. Tenth, clinicians have begun using chlorambucil as a bridge to CAR‑T therapy, shaving tumor burden enough to improve cellular product efficacy. Eleventh, patient adherence can be boosted with simple tools like smartphone alarms and pill organizers. Twelfth, caregivers report that the ability to give medication at home restores a slice of normal family routine, which is priceless for mental health. Thirteenth, proper storage-cool, dry, out of reach of pets-preserves tablet potency throughout the treatment cycle. Fourteenth, the drug’s half‑life aligns nicely with the typical 3‑4‑week treatment windows, offering flexibility in scheduling. Fifteenth, educational resources now include printable charts that demystify dosing calculations for parents. Finally, as we look toward the next decade, chlorambucil stands as a resilient pillar in the pediatric oncology toolbox, ready to adapt and support newer therapies while remaining affordable and accessible.
Tiffany Davis
January 9, 2026 AT 10:13I agree that the oral formulation simplifies logistics, and coordinating with the school nurse early can prevent unexpected absences. Sharing a clear medication plan with teachers also eases concerns about infection risk.
Don Goodman-Wilson
January 19, 2026 AT 06:20Oh great, another chemo pill to pop like candy-because what kids really need is more reasons to feel like a walking pharmacy. Sure, let’s just add another oral agent to the regimen and hope the side‑effects magically disappear.
Bret Toadabush
January 29, 2026 AT 02:26What they don’t tell you is that big pharma pushes chlorambucil to keep the cheap drug market alive while hiding newer, supposedly safer options behind patents. The whole system is rigged so families stay dependent on outdated meds that are easy to control.
Iris Joy
February 7, 2026 AT 22:33Stay strong and keep the communication lines open with your oncology team; regular labs and honest symptom reporting are the keys to navigating chlorambucil safely. Remember, you’re not alone in this journey.
Tammy Sinz
February 17, 2026 AT 18:40From a pharmacodynamic standpoint, the alkylating mechanism of chlorambucil induces interstrand cross‑links that impede replication fork progression, but how does this synergize at the molecular level with concurrent PARP inhibition in relapsed ALL? Detailed mechanistic studies could illuminate potential biomarkers for response.